CIGNA Dental Benefit Summary
Government of the District of Columbia
PPO Core Network
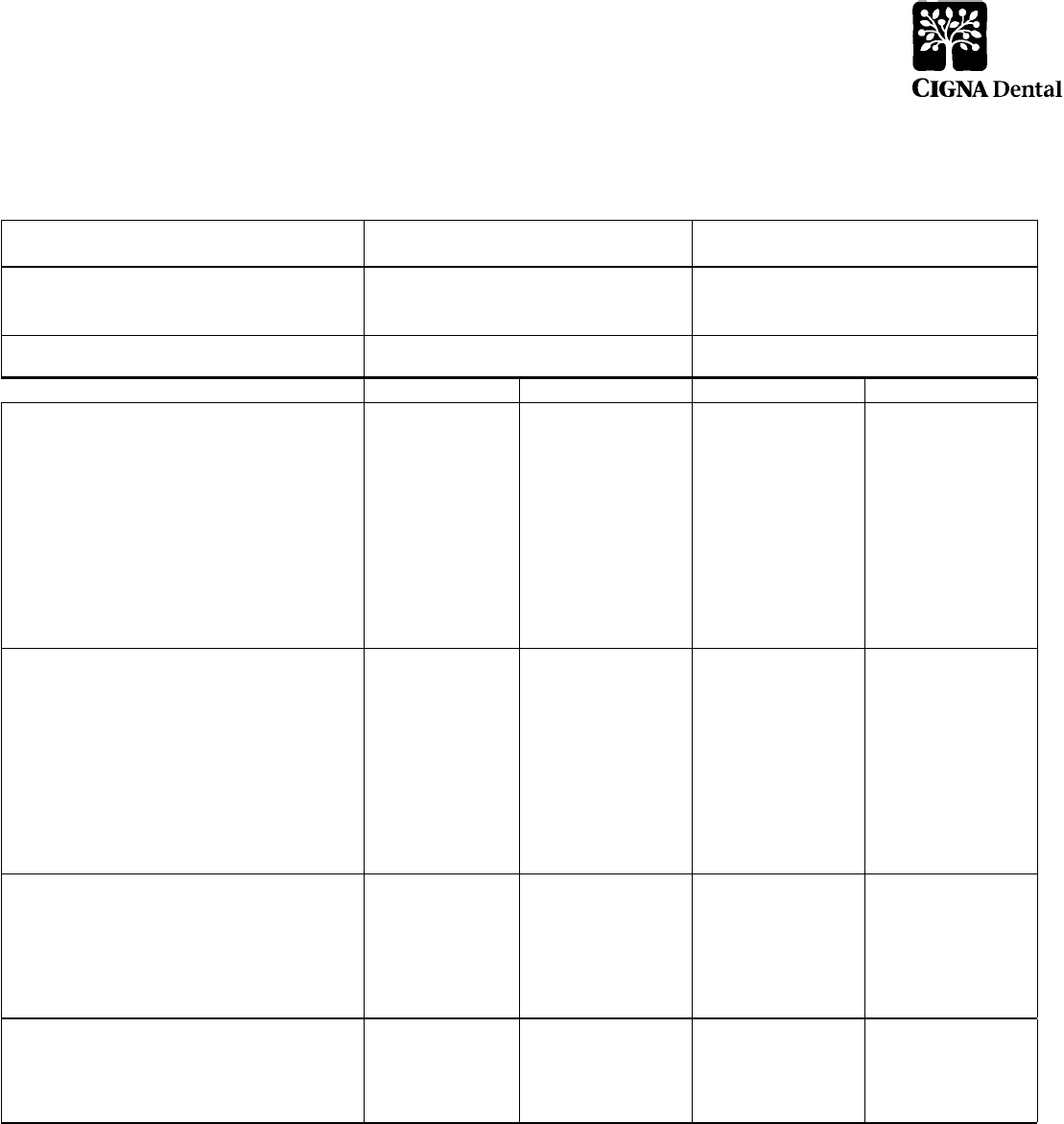
All deductibles, plan maximums, and service specific maximums (dollar and occurrence) cross accumulate between in and out of network.
Benefits CIGNA Dental PPO
In-Network Out-of-Network
Calendar Year Maximum
(Class I, II and III expenses)
$3,500 $3,500
Annual Deductible
Individual
None None
Family
None None
Reimbursement Levels
**
Based on Reduced Contracted Fees 80th percentile of Reasonable and Customary
Allowances
Plan Pays You Pay Plan Pays You Pay
Class I - Preventive & Diagnostic Care
Oral Exams
Routine Cleanings
Full Mouth X-rays
Bitewing X-rays
Panoramic X-ray
Periapical X-rays
Fluoride Application
Sealants
Space Maintainers
Emergency Care to Relieve Pain
Histopathologic Exams
100% No Charge 90% 10%
Class II - Basic Restorative Care
Fillings
Root Canal Therapy/Endodontics
Osseous Surgery
Periodontal Scaling and Root Planing
Denture Adjustments and Repairs
Oral Surgery – Simple Extractions
Oral Surgery – all except simple extractions
Anesthetics
Surgical Extractions of Impacted Teeth
Repairs to Bridges, Crowns and Inlays
90% 10% 80% 20%
Class III - Major Restorative Care
Crowns
Surgical Implants
Dentures
Bridges
Inlays/Onlays
Prosthesis Over Implant
70% 30% 50% 50%
Class IV - Orthodontia
70% 30% 50% 50%
Lifetime Maximum $3,500 $3,500
Dependent children
to age 25
Dependent children to
age 25
There is no missing tooth limitation included in the plan(s).
Pretreatment review is available on a voluntary basis when extensive dental work in excess of $200 is proposed.
**For services provided by a CIGNA Dental PPO network dentist, CIGNA Dental will reimburse the dentist according to a Contracted Fee Schedule. For services
provided by an out-of-network dentist, CIGNA Dental will reimburse according to Reasonable and Customary Allowances but the dentist may balance bill up to their
usual fees.

CIGNA Dental PPO Exclusions and Limitations
Procedure Exclusions and Limitations
Late Entrants Limit 50% coverage on Class III and IV for 12 or 24 months
Exams Two per Calendar year
Prophylaxis (Cleanings) Two per Calendar year
Fluoride 1 per Calendar year for people under 19
Histopathologic Exams Various limits per Calendar year depending on specific test
X-Rays (routine) Bitewings: 2 per Calendar year
X-Rays (non-routine) Full mouth: 1 every 36 consecutive months., Panorex: 1 every 36 consecutive months
Model Payable only when in conjunction with Ortho workup and extensive Perio treatment
Minor Perio (non-surgical) Various limitations depending on the service
Perio Surgery Various limitations depending on the service
Crowns and Inlays Replacement every 5 years
Bridges Replacement every 5 years
Dentures and Partials Replacement every 5 years
Relines, Rebases Covered if more than 6 months after installation
Adjustments Covered if more than 6 months after installation
Repairs - Bridges Reviewed if more than once
Repairs - Dentures Reviewed if more than once
Sealants Limited to posterior tooth. One treatment per tooth every three years
Space Maintainers Limited to non-Orthodontic treatment
Prosthesis Over Implant 1 per 60 consecutive months is unserviceable and cannot be repaired. Benefits are based on the amount payable for
non-precious metals. No porcelain or white/tooth colored material on molar crowns or bridges
Alternate Benefit When more than one covered Dental Service could provide suitable treatment based on common dental standards, CG will
determine the covered Dental Service on which payment will be based and the expenses that will be included as Covered
Expenses. Resins on posterior teeth will be excluded from Alternate Benefits.
Benefit Exclusions:
• Services performed primarily for cosmetic reasons
• Replacement of a lost or stolen appliance
• Replacement of a bridge or denture within five years following the date of its original installation
• Replacement of a bridge or denture which can be made useable according to accepted dental standards
• Procedures, appliances or restorations, other than full dentures, whose main purpose is to change vertical dimension, diagnose or treat conditions of TMJ, stabilize
periodontally involved teeth, or restore occlusion
• Veneers of porcelain or acrylic materials on crowns or pontics on or replacing the upper and lower first, second and third molars
• Bite registrations; precision or semi-precision attachments; splinting
• Instruction for plaque control, oral hygiene and diet
• Dental services that do not meet common dental standards
• Services that are deemed to be medical services
• Services and supplies received from a hospital
• Charges which the person is not legally required to pay
• Charges made by a hospital which performs services for the U.S. Government if the charges are directly related to a condition connected to a military service
• Experimental or investigational procedures and treatments
• Any injury resulting from, or in the course of, any employment for wage or profit
• Any sickness covered under any workers' compensation or similar law
• Charges in excess of the reasonable and customary allowances
• To the extent that payment is unlawful where the person resides when the expenses are incurred;
• Procedures performed by a Dentist who is a member of the covered person's family (covered person's family is limited to a spouse, siblings, parents, children,
grandparents, and the spouse's siblings and parents);
• For charges which would not have been made if the person had no insurance;
• For charges for unnecessary care, treatment or surgery;
• To the extent that you or any of your Dependents is in any way paid or entitled to payment for those expenses by or through a public program, other than
Medicaid;
• To the extent that benefits are paid or payable for those expenses under the mandatory part of any auto insurance policy written to comply with a“no-fault”
insurance law or an uninsured motorist insurance law. Connecticut General Life Insurance Company will take into account any adjustment option chosen under
such part by you or any one of your Dependents.
• In addition, these benefits will be reduced so that the total payment will not be more than 100% of the charge made for the Dental Service if benefits are provided
for that service under this plan and any medical expense plan or prepaid treatment program sponsored or made available by your Employer.
This benefit summary highlights some of the benefits available under the proposed plan. A complete description regarding the terms of coverage, exclusions
andlimitations, including legislated benefits, will be provided in your insurance certificate or plan description. Benefits are insured and/or administered by Connecticut
General Life Insurance Company.
CIGNA Dental refers to the following operating subsidiaries of CIGNA Corporation: Connecticut General Life Insurance Company, and CIGNA Dental Health, Inc.,
and its operating subsidiaries and affiliates. The CIGNA Dental Care plan is provided by CIGNA Dental Health Plan of Arizona, Inc., CIGNA Dental Health of
California, Inc., CIGNA Dental Health of Colorado, Inc., CIGNA Dental Health of Delaware, Inc., CIGNA Dental Health of Florida, Inc., a Prepaid Limited Health
Services Organization licensed under Chapter 636, Florida Statutes, CIGNA Dental Health of Kansas, Inc. (Kansas and Nebraska), CIGNA Dental Health of Kentucky,
Inc., CIGNA Dental Health of Maryland, Inc., CIGNA Dental Health of Missouri, Inc., CIGNA Dental Health of New Jersey, Inc., CIGNA Dental Health of North
Carolina, Inc., CIGNA Dental Health of Ohio, Inc., CIGNA Dental Health of Pennsylvania, Inc., CIGNA Dental Health of Texas, Inc., and CIGNA Dental Health of
Virginia, Inc. In other states, the CIGNA Dental Care plan is underwritten by Connecticut General Life Insurance Company or CIGNA HealthCare of Connecticut, Inc.
and administered by CIGNA Dental Health, Inc. The term “DHMO” is used to refer to product designs that may differ by state of residence of enrollee, including but
not limited to, prepaid plans, managed care plans, and plans with open access features.The CIGNA Dental PPO is underwritten and/or administered by Connecticut
General Life Insurance Company with network management services provided by CIGNA Dental Health, Inc. For Arizona/Louisiana residents the dental PPO plan is
known as CG Dental PPO. In Texas, CIGNA Dental's network-based indemnity plan is known as CIGNA Dental Choice. The CIGNA Traditional plan is underwritten
or administered by Connecticut General Life Insurance Company. In Arizona and Louisiana, the CIGNA Traditional plan is referred to as CG Traditional.
BSD21755 © 2010 CIGNA
