
Emergency First Aid Guidelines for
California Schools
Emergency Medical Services Authority
California Health and Human Services Agency
EMSA #196
Original 1994
Revised 2004
Revised 2013

Emergency First Aid Guidelines for California Schools ii
Special Recognition
Ohio Department of Public Safety, Division of EMS, EMS for Children Program;
North Dakota EMS for Children Program
Emergency First Aid Guidelines for Schools - Pilot Project Staff (First Version)
Les Gardina, MSN, RN, EMSC Coordinator, County of San Diego EMS
Cynthia Frankel, RN, EMSC Coordinator, Alameda County EMS
Kris Helander-Daughtery, RN, BSN, Prehospital Care Coordinator, Alameda County EMS
Acknowledgements
We would like to thank the following for their review and contributions to the development of these
guidelines:
County of San Diego School Nurse Resource Group
California EMSC Technical Advisory Committee
California EMSC Coordinators Group
San Diego Unified School District
Jim Harley, MD, San Diego Chapter of American Academy of Pediatrics, COPEM
Chris Riccitelli, RN, School Nurse Program Specialist, San Diego Office of Education
Barbara Muller, Coordinator for Bay Region IV, Alameda County Office of Education
Terri Christofk, Shannon Brandt, Jan Bagdasar, Meg Pesavento, San Marcos Unified
Frank De Luca, Chula Vista Elementary School
Anita Gillchrist, RN, School Nurse, San Ysidro Elementary
Stacy Hanover, RN, ED Supervisor, Children’s Hospital, Oakland, CA
Ruth Hawkins, RN, School Nurse, Encinitas Union Elementary
Patricia Murrin, RN, MPH, EMS Coordinator, County of San Diego EMS
Dale Parent, Chula Vista Elementary School
James E. Pointer, MD, Medical Director, Alameda County EMS
Mary Rutherford, MD, Director ED, Children’s Hospital, Oakland, CA
Augusta Saulys, MD, Emergency Department, Children’s Hospital, Oakland, CA
Pat Stalcup, RN, School Nurse, Ramona Unified
Gary Vilke, MD, Medical Director, County of San Diego EMS
EMERGENCY FIRST AID GUIDELINES FOR
CALIFORNIA SCHOOLS - 2013 EDITION
The San Diego project developed these guidelines with “Funding provided by the State of California Emergency Medical
Services (EMS) Authority under Special Project Grant #EMS-1055 and EMS-2062.”
Funding for the Ohio project was supported by project MCH #394003-0 from the Emergency Medical Services for Children
Program (Section 1910, PHS Act), Health Resources and Services Administration, Maternal and Child Health Bureau and
the National Highway Traffic Safety Administration.

Emergency First Aid Guidelines for California Schools iii
Acknowledgements
EMS for Children Technical Advisory Subcommittee
Erin Dorsey, RN School Nurse
Huntington Beach High School
Cynthia Frankel, RN, MSN Prehospital Care Coordinator
Alameda County EMS Agency
Marianne Gauche-Hill, MD, FACEP, FAAP Professor of Medicine
David Geffen School of Medicine at UCLA
Director of EMS
Harbor-UCLA Medical Center
Nancy McGrath, RN, MN, CPNP Pediatric Liaison Nurse
Harbor UCLA Medical Center
California Emergency Medical Services Authority
Howard Backer, MD, MPH, FACEP Director
Farid Nasr, MD Specialty Care Systems Specialist
Sandy Salaber Associate Health Program Adviser
Tonya Thomas EMS for Children Program Coordinator
California Department of Education
Gordon Jackson Assistant Superintendent
Tom Herman Education Administrator
San Joaquin County Office of Education
Cheri Coburn, Ed.D, MS, RN Director of Comprehensive Health Programs
Sacramento State University
Jan Sampson, RN, DNP, CNE Associate Professor
School of Nursing
The EMS Authority would like to acknowledge and express appreciation for the support of the
EMS for Children Technical Advisory Committee. List of committee members:
http://www.emsa.ca.gov/tech_committee

Emergency First Aid Guidelines for California Schools
ABOUT THE GUIDELINES ....................................................................................................................... 4
HOW TO USE THE EMERGENCY GUIDELINES ..................................................................................... 6
KEY TO SHAPES & COLORS .................................................................................................................. 7
EMERGENCY PROCEDURES ................................................................................................................. 8
9-1-1 GUIDELINES FOR SCHOOLS ........................................................................................................ 9
WHEN TO CALL EMERGENCY MEDICAL SERVICES (9-1-1) .............................................................. 10
DEVELOPING AN EMERGENCY PLAN ................................................................................................. 11
PLANNING FOR PERSONS WITH SPECIAL NEEDS ............................................................................ 12
MEDICATION ADMINISTRATION in SCHOOL SETTINGS .................................................................... 13
INFECTION CONTROL .......................................................................................................................... 16
ALLERGIC REACTION ........................................................................................................................... 17
.................................................................................. 18
.............................................................................................................. 19
BITES (HUMAN & ANIMAL) .................................................................................................................... 20
.................................................................................................................... 21
BITES & STINGS (MARINE) ................................................................................................................... 22
BITES & STINGS (SNAKE) ..................................................................................................................... 23
.............................................................................................................................................. 24
............................................................................................................... 25
................................................................................................................................................ 26
................................................................................................................................................... 27
CPR ........................................................................................................................................................ 29
AUTOMATED EXTERNAL DEFIBRILLATORS (AED) ....................................................................... 30
............................................................................................................................ 31
............................................................................ 32
CHOKING ............................................................................................................................................... 33
CHEST PAIN – (Heart Attack) ................................................................................................................. 34
CHILD ABUSE & NEGLECT ................................................................................................................... 35
COMMUNICABLE DISEASES ................................................................................................................ 36
DIABETES .............................................................................................................................................. 37
TABLE OF CONTENTS

Emergency First Aid Guidelines for California Schools 2
DIARRHEA ............................................................................................................................................. 38
DROWNING/NEAR DROWNING ............................................................................................................ 39
EARS ...................................................................................................................................................... 40
ELECTRICAL INJURY ............................................................................................................................ 41
EYES (INJURY) ...................................................................................................................................... 42
FAINTING ............................................................................................................................................... 44
FEVER & NOT FEELING WELL ............................................................................................................. 45
FINGERNAIL/TOENAIL INJURY ............................................................................................................. 46
FRACTURES, DISLOCATIONS, SPRAINS OR STRAINS ...................................................................... 47
FROSTBITE ............................................................................................................................................ 48
HEAD INJURIES ..................................................................................................................................... 49
HEADACHE ............................................................................................................................................ 50
HEAT EXHAUSTION/HEAT STROKE .................................................................................................... 51
HYPOTHERMIA (EXPOSURE TO COLD) .............................................................................................. 52
LOSS OF CONSCIOUSNESS ................................................................................................................ 53
MENSTRUAL PROBLEMS ..................................................................................................................... 54
MOUTH & JAW INJURIES ...................................................................................................................... 55
NECK & BACK PAIN ............................................................................................................................... 56
NOSE ...................................................................................................................................................... 57
POISONING & OVERDOSE ................................................................................................................... 59
PREGNANCY ......................................................................................................................................... 60
RASHES ................................................................................................................................................. 61
SEIZURES .............................................................................................................................................. 62
SERIOUSLY ILL/SHOCK ........................................................................................................................ 63
SPLINTERS or IMBEDDED PENCIL LEAD ............................................................................................ 64
STOMACH ACHES/PAIN ........................................................................................................................ 65
SUICIDE (See BEHAVORIAL EMERGENCIES)
TEETH & GUMS ..................................................................................................................................... 66
TETANUS IMMUNIZATION .................................................................................................................... 68
TICKS ..................................................................................................................................................... 69
VOMITING .............................................................................................................................................. 70
TABLE OF CONTENTS

Emergency First Aid Guidelines for California Schools 3
WOUNDS (CUTS, SCRATCHES & SCRAPES INCLUDING ROPE & FLOOR BURNS) ......................... 71
WOUNDS (PUNCTURE) ......................................................................................................................... 72
WOUNDS (STABS & GUNSHOT) ........................................................................................................... 73
RECOMMENDED FIRST AID EQUIPMENT AND SUPPLIES FOR SCHOOLS ...................................... 74
EMERGENCY PHONE NUMBERS ......................................................................................................... 75
TABLE OF CONTENTS

Emergency First Aid Guidelines for California Schools 4
The Emergency First Aid Guidelines for California Schools’ document was initially developed by
San Diego and Alameda Counties, funded in part by a grant from the California Emergency
Medical Services (EMS) Authority. The Guidelines were originally based on the second edition
of the Ohio Emergency Guidelines for Schools, 2000. The Emergency First Aid Guidelines for
California Schools manual is meant to provide recommended procedures for school staff in
responding to medical emergencies when the school nurse is not available and until emergency
medical services responders arrive on scene. These guidelines provide recommended actions
and do not supersede or invalidate any laws or rules established by a school system, a school
board, or the State.
Due to declining school district budgets, school nurses are not always present on school
grounds when medical emergencies occur. It is not uncommon to have a school nurse present
for only two hours a week per campus. Currently, only fifty percent (50%) of school districts in
California have a school nurse on staff. The Emergency First Aid Guidelines for California
Schools was developed over a two-year period and piloted in thirteen schools in San Diego
County and three schools in Alameda County. They were enthusiastically received in the pilot
areas by school nurses and educators as a layperson’s emergency medical reference tool.
Once the pilot projects were completed, the draft Guidelines were reviewed and revised by the
local Emergency Medical Services for Children (EMSC) Coordinators Group and the EMSC
Technical Advisory Committee (TAC). Extensive comments and revisions were made by these
committees. The EMSC Coordinators Group is composed of local EMSC program managers
and the TAC membership is composed of emergency physicians, nurses, prehospital and
administrative experts in EMSC. The EMSC TAC first approved the draft Guidelines during its
January 29, 2004 meeting and forwarded the document to the EMS Authority for review and
approval.
During the first revision of the Guidelines document in 2004, the EMS Authority collaborated with
the California Department of Education and the California School Nurses Association. The
revised Emergency First Aid Guidelines for California Schools’ document was sent out for a 30-
day public comment period from April 16, 2004 to May 17, 2004. Comments and suggested
revisions received have been incorporated into the Guidelines and/or responded to as
appropriate. The Emergency First Aid Guidelines for Schools document was approved on June
23, 2004 by the Commission on EMS. One hard copy and a CD of the Guidelines were
distributed to approximately 10,000 California schools.
The current version, the second revision, is based on 2010 American Heart Association
Guidelines for CPR and ECC, which was approved by the EMSC TAC and EMSC Coordinators
Group on January 26-27, 2012.
ABOUT THE GUIDELINES

Emergency First Aid Guidelines for California Schools 5
Please take some time to familiarize yourself with the format and review the “How to Use the
Guidelines” section on page 6 prior to an emergency situation. The guidelines are
recommended procedures for when advanced medically trained personnel are not available on
the school site. It is strongly recommended that staff who are in a position to provide first
aid to students complete an approved first-aid and cardiopulmonary resuscitation (CPR)
course. Please consult your school nurse if you have any questions concerning the
recommendations contained in the guidelines.
These guidelines should not delay calling 9-1-1 in the event of an emergency.
Periodically, the EMS Authority may send out updates on procedures dealing with the medical
emergencies that are in the guidelines. When received, please remove the old information and
replace with the updated information.
We welcome comments, suggestions, or experiences using these guidelines.
Email address: [email protected]
ABOUT THE GUIDELINES (CONT.)

Emergency First Aid Guidelines for California Schools 6
The last page of this document provides space for important emergency phone numbers in your
area. It is important to complete this information, when you receive the document, to have this
information ready in an emergency situation.
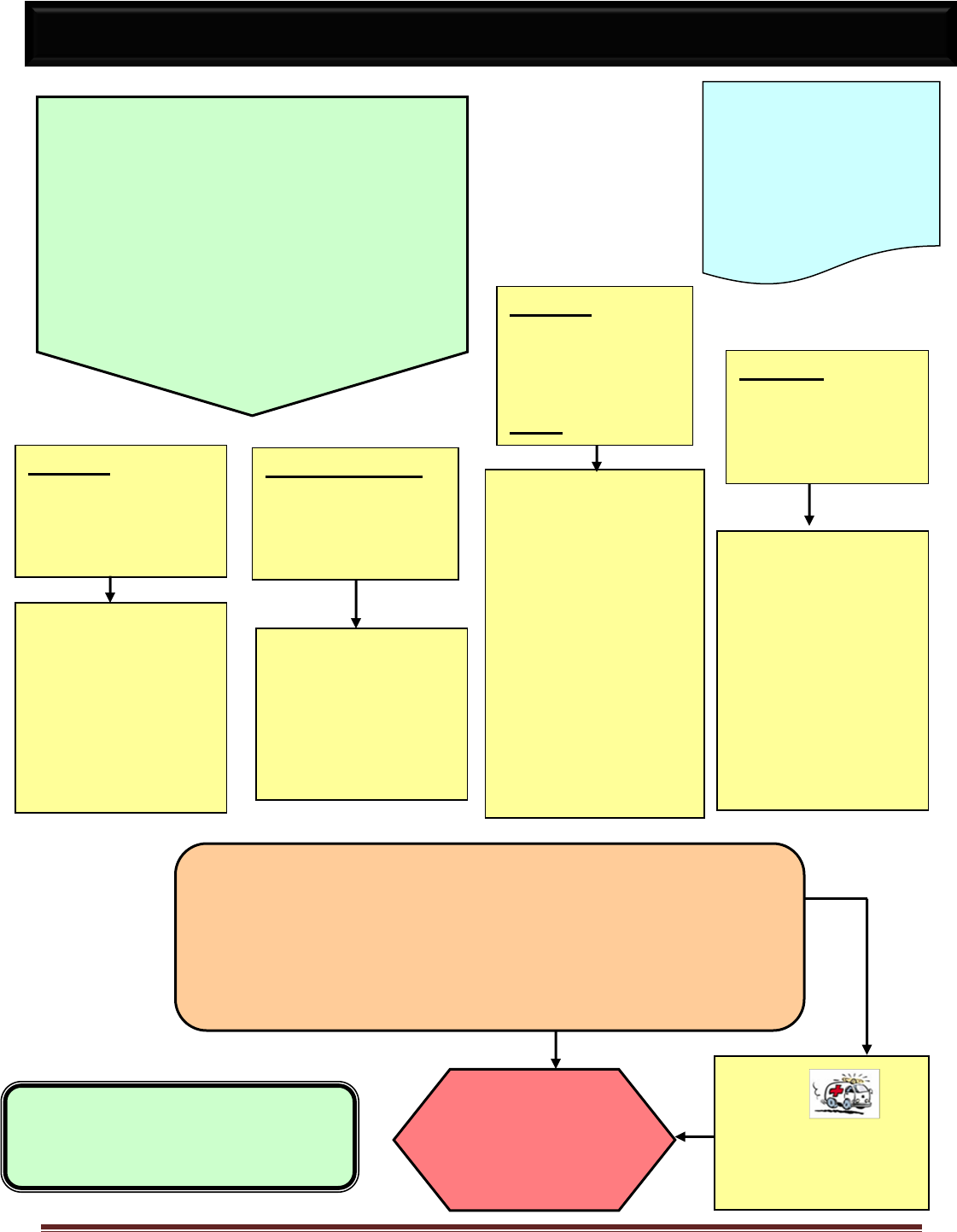
A colored flow chart format is used to guide you easily through all symptoms and management
steps from beginning to end. See the Key to Shapes and Colors (pg. 7).
Emergency Procedures for an Injury or Illness section (pg. 8) gives a general overview of the
recommended steps in an emergency situation and the safeguards that should be taken.
Additional information includes when to call EMS (pg. 10), developing a school wide emergency
plan (pg. 11), infection control procedures (pg. 12), and planning for persons with special
healthcare needs (pg. 12).
If medical assistance is needed, have someone contact the 9-1-1 system as soon as possible.
HOW TO USE THE EMERGENCY GUIDELINES

Emergency First Aid Guidelines for California Schools 7
This note provides
background information.
This type of box should be
read before emergencies
occur.
YES
NO
Initial Information, questions, actions
Provides First-Aid
Instructions
START
HERE
KEY TO SHAPES & COLORS
? Question Being Asked?
You need to choose based on
person’s condition or response.
Follow the pathway for your answer.
Additional Information
STOP HERE
This is the final
instruction

Emergency First Aid Guidelines for California Schools 8
1. Remain calm and assess the situation. Be sure the situation is safe for you to
approach. The following dangers will require caution: live electrical wires, gas leaks,
chemical exposure, building damage, unstable structures, fire or smoke, traffic,
agitated or violent students.
2. A responsible adult should stay at the scene and give help until the person
designated to handle emergencies arrives. For serious injury or illness, call 9-1-1
without delay.
3. Notify the responsible school nurse or administrator designated to handle
emergencies. Upon arrival this person should take charge of the emergency.
4. Do NOT give medications unless there has been prior written approval by the
person’s parent or legal guardian and doctor. Administer medications according to
local school board policy and state or federal laws and regulations.
5. Do NOT move a severely injured or ill person unless absolutely necessary for
immediate safety. If moving is necessary, protect the neck by keeping it straight to
prevent further injury, see the “Neck and Back Pain” guideline (pg. 56).
6. Call Emergency Medical Services (EMS 9-1-1), if appropriate, or arrange for
transportation of the ill or injured person, if necessary. Provide EMS personnel with
copies of physician/parents’ signed record of medical instructions for emergencies
(i.e., pupil emergency card).
7. The responsible school nurse, administrator, or a designated employee should notify
the parent/legal guardian of the emergency as soon as possible to determine the
appropriate course of action.
8. If the parent/legal guardian cannot be reached, notify a parent/legal guardian
substitute and call either the physician or the hospital designated on the Emergency
Information Card, so they will know to expect the injured or ill person.
9. Each person should have an emergency information record (i.e., student emergency
card) on file that provides essential contact information, medical conditions,
medications and an emergency care plan if appropriate. Provide a copy of student’s
emergency information to EMS upon arrival, if authorized by parent/legal guardian.
10. Fill out a report for all injuries and illnesses requiring above procedures if indicated
by school policy.
EMERGENCY PROCEDURES
FOR INJURY OR ILLNESS

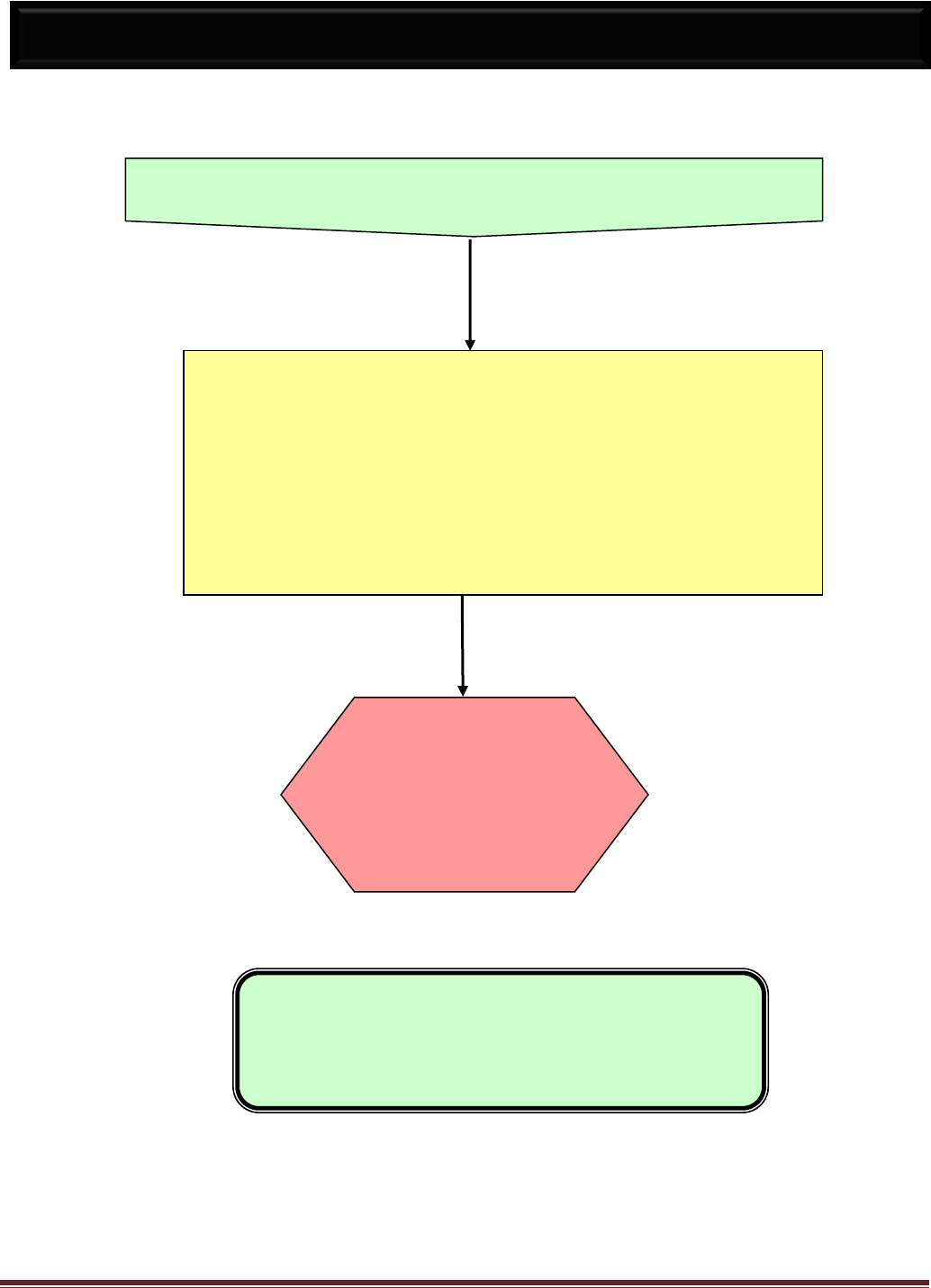
Emergency First Aid Guidelines for California Schools 9
CALL 9-1-1 FOR:
Difficulty Breathing Caused by
Absent or labored breathing (pg. 32)
Choking (pg. 33)
Wheezing due to allergic reaction
Near drowning (pg. 39)
After bee sting (pg. 17)
Loss of Consciousness (pg. 53)
For any reason, including
After any injury
With history of diabetes
After seizure
Unexplained reason
Uncontrolled Bleeding (pg. 24)
Head Injury with (pg. 49)
Severe headache
Vomiting
Change in Behavior
Possible Poisoning (pg. 59)
IF IN DOUBT - CALL 9-1-1
9-1-1 GUIDELINES FOR SCHOOLS
Call 911 Immediately
Verify address
Answer Questions
Follow Instructions
Do Not Hang Up
Stay Calm
Provide First Aid
until ambulance
arrives
These guidelines are not intended to limit good judgment in emergency situations!
9-1-1 brings medical professionals to the scene of the emergency.
Delays in accessing the 9-1-1 system can cause harm to the injured. Consult your
local policies on the management of health emergencies.

Emergency First Aid Guidelines for California Schools 10
Call EMS if:
The person is not breathing.
The person is having difficulty breathing, shortness of breath or is choking.
The person has no pulse.
The person is unconscious, semi-conscious or unusually confused.
The person has bleeding that won’t stop.
The person is coughing up or vomiting blood.
The person has chest pain or pressure persisting more than 3-5 minutes, or has
chest pain that goes away and comes back.
The person has been poisoned or taken an overdose.
The person has a seizure for the first time, a seizure that lasts more than
5 minutes, multiple seizures, or has a seizure and is pregnant or diabetic.
The person has received anti-seizure medication as allowed under the provisions
of Education Code Section 49414.7.
The person has injuries to the head, neck or back.
The person has sudden, severe pain anywhere in the body.
The person has an open wound over a suspected fracture or where bone or
muscle is exposed.
The person’s condition is limb-threatening or other injuries that may leave the
person permanently disabled unless he/she receives immediate care; for example:
lack of feeling or normal color on injured limb (arm or leg); amputation; severe eye
injury or chemical exposure to the eye.
Moving the person could cause further injury.
The person needs the skills or equipment of paramedics or emergency medical
technicians.
Distance or traffic conditions would cause a delay in getting the person to the
hospital.
If any of the above conditions exist, or if you are not sure, it is best to call
EMS (9-1-1).
Sources: American Red Cross & American College of Emergency Physicians
WHEN TO CALL EMERGENCY MEDICAL SERVICES
(9-1-1)

Emergency First Aid Guidelines for California Schools 11
A school-wide emergency plan should be developed in cooperation with school health staff, school
administrators, local EMS, local hospital, local health department and parent/guardian organizations.
All employees should be trained on the emergency plan and a written copy should be available at all
times. The plan should be reviewed and updated annually, and should consider the following:
Staff roles are clearly defined in writing. For example, staff responsibility for rendering care,
accessing EMS, notifying responsible school administrator and parents, and supervising
uninjured children are outlined and practiced. A responsible administrator for emergency
situations has been designated within each school. In-service training is provided to maintain
knowledge and skills for employees designated to respond to emergencies.
At least one individual, other than the nurse, is trained in CPR and first aid in each school.
Teachers and employees working in high-risk areas or activities (e.g., labs, gyms, shops, P.E.,
etc.) are trained in CPR, use of AED, and first aid.
With appropriate staff training, these First Aid Guidelines could be utilized by staff for immediate
care of students. The Guidelines are to be distributed or available to appropriate employees.
Files are in order for each student and are kept in a central location. The files should contain
current emergency contact and authorization information, immunization and medical records,
phone number of student’s doctor, medication administration forms and emergency care plans
for students with special needs.
First aid kits are stocked with up-to-date supplies and are available in central locations, high-risk
areas, and for extracurricular activities. See “Recommended First Aid Supplies” (pg. 74)
All employees have rapid access to emergency numbers. Emergency numbers are available and
posted by phones. See “Emergency Phone Numbers” (pg. 75)
School personnel have communicated with local EMS regarding the emergency plan, services
available, persons with special needs and other pertinent information about the school.
A written policy describes procedures for accessing EMS without delay from all locations (e.g.,
playgrounds, athletic fields, fieldtrips, extracurricular activities, etc.).
A written policy that provides instructions for transportation of an injured or ill student.
Considerations and procedures for a person with special needs. See “Planning for Persons with
Special Needs” (pg. 12)
A doctor or school nurse and a dentist are designated to act as consultants to the school for
health and safety related questions. (Education Code 44871-44878)
All injuries are documented in a standard format and maintained in an organized manner. Injury
reports are reviewed on a regular basis to revise the emergency plan and remedy hazards.
DEVELOPING AN EMERGENCY PLAN

Emergency First Aid Guidelines for California Schools 12
PLANNING FOR PERSONS WITH SPECIAL NEEDS
Some persons in your school may have special emergency care needs due to their
medical conditions or functional needs.
Medical Conditions:
Some persons may have special or chronic conditions that put them at risk for serious or life-
threatening emergencies. For example, persons who have:
Seizures
Life-threatening or severe allergic reactions
Diabetes
Technology-dependent or medically fragile conditions
Your school nurse or other duly qualified supervisor of health, along with the person’s parent or
legal guardian and personal physician, should develop individual emergency care plans for
these persons when they are enrolled. These emergency care plans should be made available
to appropriate staff at all times. In the event of an emergency situation, refer to the person’s
emergency care plan. The American College of Emergency Physicians (ACEP) and the
American Academy of Pediatrics (AAP) have created an Emergency Information Form for
Children with Special Needs. It can be downloaded from www.aap.org or www.acep.org.
Physical Abilities:
Other persons in your school may have special emergency needs due to physical disabilities.
For example, persons who are:
Deaf
Blind
In wheel chairs or using other assistive devices
Unable or have difficulty walking up or down stairs
Temporarily on crutches
These persons will need special arrangements in the event of a school-wide emergency (e.g.,
fire, tornado, earthquake, building collapse, evacuation, etc.).
A plan should be developed and a responsible person should be designated to
assist these persons and staff to safety. All appropriate staff should be aware of
this plan.

Emergency First Aid Guidelines for California Schools 13
A significant and growing number of school children have health problems that require the
administration of medication during the school day. There are several reasons why students
might require medications in schools, including: (1) chronic conditions requiring medication in
order to benefit from classroom instruction; (2) acute, but temporary, medical needs that require
medicine during the school day, such as an antibiotic for an infection; or (3) conditions that might
require emergency medication, such as an Epinephrine (Epi-pen)® for a bee sting or food
allergy.
Children who require medications in order to fully benefit from public education are protected by
federal and state disability laws. It has become a complex issue due to a variety of factors, such
as federal and state disability law, new pharmaceutical and medical technologies, evolving
mental and medical health practices, fewer full-time school nurses, and increasing numbers of
children with complex as well as simple health needs in schools.
The National Association of School Nurses states that the school nurse has the educational
background, knowledge, and licensure that provide the unique qualifications to direct the
administration of medications in the school setting. The position statement recommends that
“school districts develop policies and procedures to address medication administration in
accordance with federal and state laws and guidelines.”
1
If a child needs specified medication
during the course of the school day to attend school and benefit from the educational program; it
is in the school's interest to make this accommodation.
2
California law states
3
, with a few clearly specified legal exceptions, that only a licensed nurse or
physician may administer medication. In the school setting, these exceptions are situations
where: (1) The student self-administers the medication; (2) parent or parent designee, such as a
relative or close friend, administers the medication
4
; or (3) there is a public disaster or epidemic.
5
The Legislature has enacted four statutes that authorize unlicensed school personnel to be
trained and supervised in order to administer four specific medications in medical emergencies:
1. Under the supervision of a school nurse or physician designee, an unlicensed school
employee may administer epinephrine via auto-injector;
6
2. Under the supervision of a school nurse, physician, registered nurse, or public health
nurse, an unlicensed school employee may administer glucagon;
7
3. Under the supervision of a school nurse, physician, registered nurse, or public health
nurse, an unlicensed school employee may administer Diastat, and
8
4. Under the supervision of a school nurse, physician, registered nurse, or public health
nurse, an unlicensed school employee may administer insulin.
9
MEDICATION ADMINISTRATION
in SCHOOL SETTINGS

Emergency First Aid Guidelines for California Schools 14
In accordance with Education Code (EC) sections 49414, 49414.5 an unlicensed school
employee could "administer" epinephrine via auto-injector directly into a student suffering
anaphylaxis, glucagon via needle and syringe directly into a student suffering from severe
hypoglycemia, insulin, via needle and syringe directly into a student suffering from severe
hyperglycemia or Diastat, a medication that is administered rectally to a student with epilepsy
suffering from seizures. No other California statute allows an unlicensed school employee to
administer any other medication in California public schools, even if the unlicensed school
employee is trained and supervised by a school nurse or other similarly licensed nurse.
EC Section 49423 permits the school nurse or other designated school personnel to "assist"
students who must "take" medication during the school day that has been prescribed for that
student by his or her physician. The terms “assist” and “administer” are not synonymous. An
example of an unlicensed school employee “assisting” a student pursuant to EC Section 49423
would be when the school employee removes the cap from the medication bottle, pours out the
prescribed dose into a cup or a spoon, and hands the cup or spoon to the student, who then
"takes" or self-administers the required medication. With the above-stated statutory exceptions,
there is no clear statutory authority in California permitting that same unlicensed school
employee to "administer” any other medication.
PROGRAM ADVISORY ON MEDICATION ADMINISTRATION
10
CCR Title 5 601-611: California Department of Education “Program Advisory on Medication
Administration” (2005, reviewed 2012).
A school may administer medication to a child only if a parent or guardian has specifically
requested such action and there is a reason to administer the medication when the child is at
school. A written order from an individual who is licensed to prescribe medications must be on
file in order to administer medications. Medication may be administered at school by the school
nurse, other duly qualified supervisors of health,
11
site administrator or designee as allowed by
law. Neither the school nurse nor her designee is permitted to administer medication unless:
1. The medication is in the original properly labeled container. If it is a prescription medicine,
the student’s name, name of the drug, dosage, time for administering, and name of health
care provider and current date is printed on the container.
2. Written orders from the student's health care provider are on file in the school stating:
Student’s name
Date of Birth
Name of medication
Dosage (EC Section 49423)
Purpose of the medication
Method of administration (EC Section 49423)
Time of day medication is to be given (EC Section 49423)
Anticipated number of days it needs to be given in school and possible side effects
MEDICATION ADMINISTRATION
in SCHOOL SETTINGS (CONT.)

Emergency First Aid Guidelines for California Schools 15
3. Name, address, telephone number, and signature of the California authorized health care
provider.
4. The parent/guardian provides written permission to the school to administer a prescription
or over-the-counter medication.
5. School personnel keep an individual record of any medications administered by school
personnel.
6. Medication is stored in a clean, locked cabinet or container.
7. Written statements authorizing medications to be administered at school be renewed
yearly or whenever changes in medication or authorized health care provider occur.
8. Changes in medication authorization that generate a new written statement include the
following circumstances:
a. Changes in medication dose, time, and method of administration
b. Change in medication
c. Change in California authorized health care provider
d. Discontinuance of medication administration
Additionally, school districts may want to consider requiring parents to sign a release from
responsibility pertaining to side effects or other medical consequences that may be related to the
medication(s).
1
National Association of School Nurses. (2003). Position statement: Medication administration in the school setting.
http://www.nasn.org/positions/medication.htmv.
2
Schwab, N.C. and Gelfman, M.H.B., (2001). Legal Issues in School Health, Sun River Press, North Branch, MN: Sunrise River Press, 205.
3
California Business and Professions Code (Nursing Practice Act (NPA)) Sections 2725 and 2727 and the California Education Code.
4
NPA Section 2727(a) states that parents and other relatives or close friends may administer medication, which is defined as “gratuitous
nursing.”
5
NPA Section 2727(d) states that a district not having a school nurse does not qualify as a “public disaster.”
6
EC Section 49414
7
EC Section 49414.5
8
EC Section 49414.7 is an optional law that was signed by Governor Brown October 7, 2011 and went into effect January 1, 2012 –SB 61 (Huff).
9
EC Section 49423 provides that unlicensed school personnel may assist with medication administration; BPC 2725(b)(2) and the CCR, Title 5,
section 604 authorize specified persons to administer insulin in California’s public schools pursuant to a Section 504 Plan or an IEP.
10
California Code of Regulations Title V, Article 4.1: Administering Medication to Students or Otherwise Assisting Students in the Administration
of Medication During the Regular School Day. http:// www.cde.ca.gov/ls/he/hn/documents/medadvisory.pdf
11
Medication may be administered at school by the school nurse, other duly qualified supervisors of health, site administrator or designee as
allowed by law, the parent or guardian or their designee as allowed by law or LEA policy, a contracted licensed health care professional whose
licensure permits administration of the medication, or by the student under specified conditions. Unlicensed school personnel designated by the
site administrator administer medication if: a. The unlicensed staff member is willing to perform medication administration; b. The unlicensed
staff member is trained and determined to be capable and competent to be able to safely and accurately administer the medication by a licensed
health care professional, who is legally authorized to provide such training and determine competence; c. The unlicensed staff member
performing medication administration is supervised by the licensed health care professional who provided the training, and the supervision,
review, and monitoring of the medication administration is documented.
MEDICATION ADMINISTRATION
in SCHOOL SETTINGS (CONT.)

Emergency First Aid Guidelines for California Schools 16
To reduce the spread of infectious diseases (diseases that can be spread from one
person to another), it is important to follow Universal Precautions when providing care to
any ill or injured student, whether or not the person is known to be infectious. Universal
precautions are a set of guidelines that assume that all blood and certain other body
fluids are potentially infectious. The following list describes universal precautions:
Wash hands thoroughly with soap and water for at least 20 seconds. When
hands are visibly dirty or visibly soiled with blood or other body fluids (be sure to
scrub between fingers, under fingernails, and around the tops and palms of
hands). If hands are not visibly soiled you may use an alcohol-based hand rub.
Wash hands:
1. Before and after physical contact with any person
(even if gloves have been worn).
2. Before and after eating or handling food
3. After contact with a cleaning agent
4. After using the restroom
5. After providing any first-aid
Wear disposable gloves when in contact with blood and other body fluids.
Wear protective eyewear when body fluids may come in contact with eyes
(e.g., squirting blood).
Wipe-up any blood or body fluid spills as soon as possible (wear
disposable gloves). Double-bag the trash in plastic bags, or place in a
Ziploc bag and dispose immediately. Clean the area with an approved
disinfectant or a bleach solution (one part liquid bleach to 10 parts water).
Send all soiled clothing (i.e., clothing with blood, feces or vomit) home with the
person in a double-bagged plastic bag.
Do not eat, touch your mouth, or touch your eyes while giving any first aid.
INFECTION CONTROL
Guidelines:
Remind students to wash hands thoroughly after coming in contact with any blood or
body fluids.
.
Remind students to avoid contact with another person’s blood or body fluid.

Emergency First Aid Guidelines for California Schools 17
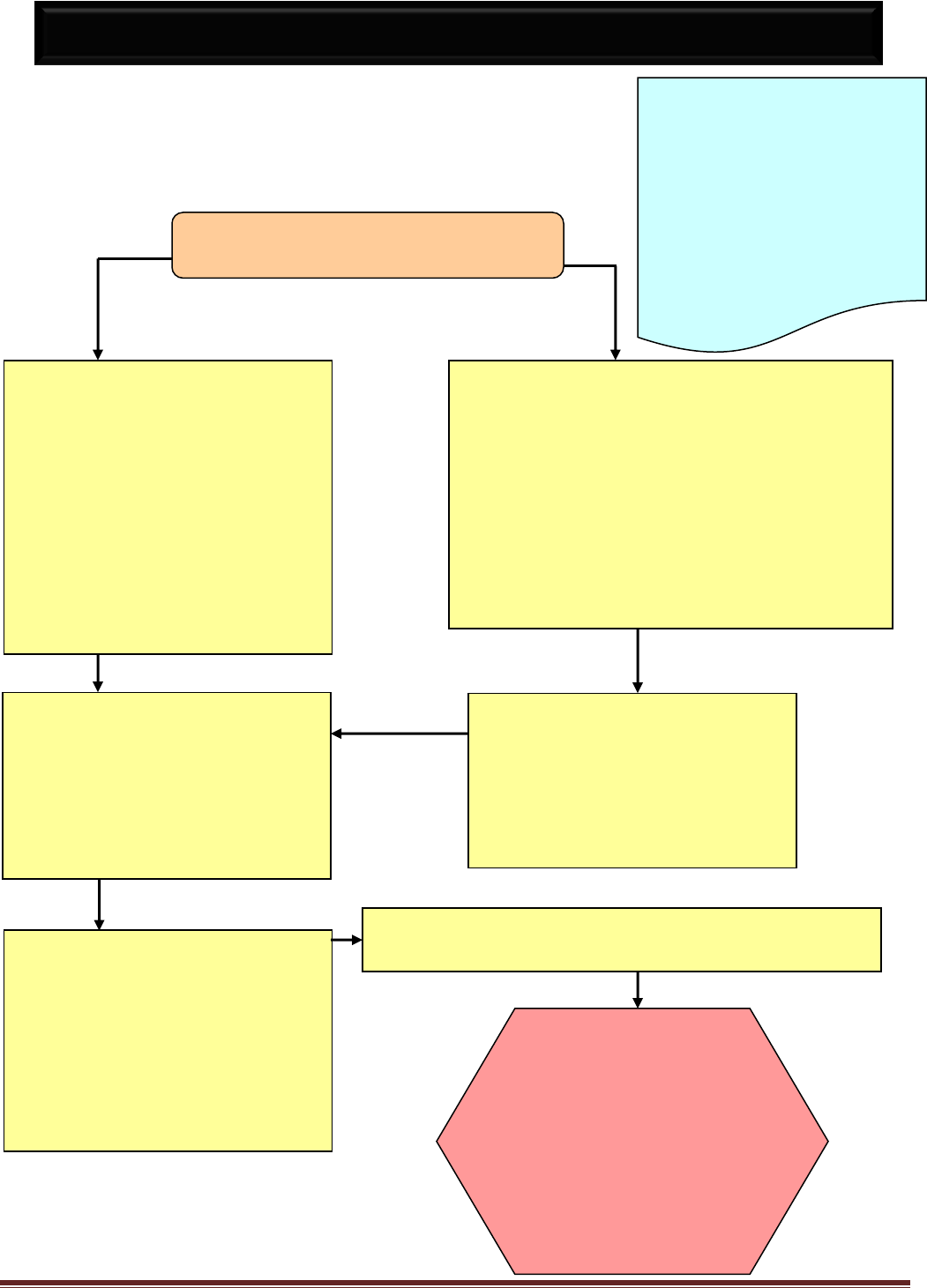
NO
NO
YES
YES
. .
Refer to Emergency Action/Care Plan, if
available
Administer Epinephrine (EpiPen) as per
school protocol
Administer other doctor and
parent/guardian-approved medication as
prescribed - CALL EMS 9-1-1
Ask if person is having difficulty breathing or swallowing
Ask person if they have a history of allergic reaction
Check for a medical bracelet or medallion
Contact responsible
school nurse or
administrator & parent
or legal guardian.
Persons with a history of
life-threatening allergies
should be known to
appropriate school staff.
An emergency care plan is
needed upon enrollment.
Staff in a position to
administer approved
medications should
receive instruction.
A person may experience a delayed allergic
reaction up to 2 hours following food or medication
ingestion, bites, bee sting or exposure to
chemicals, plants, etc.
Does the person have a history or current
symptoms of a severe allergic reaction to
the recent exposure? (see below)
ALLERGIC REACTION
Keep quiet & in position of comfort
Be prepared to use “CPR”
Is person so uncomfortable that he is
unable to participate in school
activities?
Brush off dry substances (wear gloves)
Flush contact area or substance from
skin and eyes with water
Notify adult supervising person of
exposure (bee sting or ingestion) and
possibility of delayed allergic reaction
Observe mild reactions
Review person’s emergency plan
Symptoms of a Severe Allergic Reaction after Exposure
Difficulty breathing, wheezing
Pale, gray, blue or flushed skin/lips
Difficulty swallowing, drooling
Poor circulation (See “Seriously Ill/Shock”)
Continuous coughing or sneezing
Nausea and/or vomiting
Tightening of throat or chest
Weakness, dizziness
Swelling of face, neck or tongue
Seizures
Confusion or loss of consciousness
Suddenly appears seriously sick
Generalized rash or hives
Symptoms Of A Mild Allergic Reaction
Red, watery eyes
Itchy, sneezing, runny nose
Rash or hives in local area or widely scattered
Localized swelling, redness
Return to class

Emergency First Aid Guidelines for California Schools 18
Signs of Breathing Difficulty
Rapid/Shallow breathing
Tightness in chest
Excessive coughing
Not able to speak in full sentences
Widening of nostrils
Appears very anxious
Wheezing (high pitched sound)
Increased use of stomach
and chest muscles
YES
NO
YES
NO
ASTHMA/WHEEZING/DIFFICULTY BREATHING
CALL EMS 9-1-1
May give room
temperature water to drink
Person may return to
class when recovered
Are symptoms not improving or getting worse?
Having difficulty speaking in full sentences?
Loud wheeze or persistent cough?
Decreased level of consciousness?
Persons with a history of breathing
difficulties, including asthma or
wheezing, should be known to
appropriate school staff. Develop a
school asthma action plan during
enrollment. Keep asthma inhaler and
spacer available. Student may carry
their own medication. Staff authorized
to administer medications should
receive instruction.
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
CALL EMS 9-1-1
Asthma/wheezing attacks may be triggered by many
substances/activities. Hypersensitive airways
become smaller, causing wheeze, cough, and
difficulty breathing. Attacks may be mild, moderate
or severe. Refer to emergency care plan.
Sit person upright in position of comfort
STAY CALM. Be reassuring
Ask if person has allergies or medication
Did breathing difficulty develop rapidly?
Is the student having difficulty speaking due
to shortness of breath?
Are lips, tongue or nail beds turning blue?
Change in level of consciousness-confusion?
If available, check school asthma action plan
If person has doctor and parent/guardian approved inhaler
medication, assist or administer medication as directed
Observe for 4-5 min and repeat as directed, if not improved
Encourage person to sit quietly, breathe slowly and deeply
in through the nose and out through the mouth

Emergency First Aid Guidelines for California Schools 19
NO
NO
YES
YES
See appropriate guideline to
provide first aid, if any injury
requires immediate care.
CALL EMS 9-1-1
CALL POLICE 9-1-1
Ask for a police response.
Communications should be non-threatening. Acknowledge that the person is upset,
offer to help, make eye contact, and avoid physical contact. Stay out of reach, and
ensure an accessible escape route. DO NOT challenge or argue. Attempt to involve
people who the person trusts, and talk about what is wrong. If available, have another
adult stand nearby, in a nonthreatening manner, in case student’s behavior escalates.
Check Emergency Action/Care Plan for more information.
Persons with a history of
behavioral problems,
emotional problems or
other special needs should
be known to appropriate
staff. An emergency care
plan should be developed
at time of enrollment.
Refer to your school's policy for addressing behavioral
emergencies. Behavioral or psychological emergencies
may take many forms (e.g., depression, anxiety/panic,
phobias, destructive or assaultive behavior, etc.).
Intervene only if the situation is safe for you.
Call for assistance
Are there visible injuries? Signs of
poisoning or patient has admitted to
taking medications or drugs.
Does person's behavior present an
immediate, risk of physical harm to
self, other persons or property?
Is person armed with a weapon?
Contact responsible
school nurse or
administrator and
parent or legal
guardian.
BEHAVIORAL EMERGENCIES
The cause of unusual behavior may be psychological/emotional or physical (e.g., fever,
diabetic emergency, poisoning/overdose, alcohol/drug abuse, head injury, etc.).
The person should be seen by a health care provider to determine the cause.
Suicidal and violent behavior should be taken seriously. If the person has threatened to
harm himself/herself or others, contact the responsible school authority immediately.
If needed:
Suicide Hotline
(1-800-273-8255)
www.suicideprevention
lifeline.org

Emergency First Aid Guidelines for California Schools 20
BITES (HUMAN & ANIMAL)
Wear disposable gloves
when exposed to blood
or other body fluids.
Hold bite area under running
water for 2-3 minutes
Wash with soap and water
If wound bled, apply clean
bandage
Is the person bleeding?
Maintain direct pressure
CALL 9-1-1
See “Bleeding” (pg. 24)
Press firmly with a clean
dressing/cloth on bleeding site,
see “Bleeding” (pg. 24)
Check immunization record for
DT, DPT, Tdap, or DTaP
(tetanus). See “Tetanus” (pg. 68)
for more information.
Is bite from a human?
If bite is from a snake, scorpion or other
reptile, hold the bitten area still and
below the level of the heart.
Call POISON CONTROL CENTER
1-800-222-1222
See “Snake Bite”, if appropriate (pg. 23)
If bite is from an animal:
Don’t try to catch or touch
the animal
Get description and
location of animal
Report to Animal Control
or proper authority,
usually the local Health
Department, so that
animal can be caught &
watched for rabies
Contact responsible school nurse
or administrator and parents/legal
guardian. If a human bite, inform
both the person bitten and the
person biting that they may have
been exposed to blood from
another person. If skin is broken
seek medical care.
ENCOURAGE IMMEDIATE
MEDICAL CARE
File Incident Report
Is bite large or gaping?
Is blood spurting?
Is bleeding
uncontrolled?
YES
NO
NO
YES
YES
NO
NO
YES

Emergency First Aid Guidelines for California Schools 21
Allergic reactions may be delayed up to two (2) hours
See “Allergic Reaction” for sign and symptoms (pg. 17)
Does person have symptoms of:
Difficulty breathing?
Swelling of face, tongue or neck?
Coughing or wheezing that does not stop?
History of severe allergic reactions?
Keep person quiet
See “Allergic Reaction” (pg. 17)
Position of Comfort
Be prepared to perform “CPR”
BITES & STINGS (INSECT)
Also see
Bites & Stings for:
Human (pg. 20)
Marine (pg. 22) &
Allergic Reaction (pg. 17)
Known history of allergic
reactions should be
recorded at school and
made available to all
school staff. An
emergency care plan is
needed.
Get description of insect or spider.
Did a scorpion sting person?
Call POISON
CONTROL
CENTER
1-800-222-1222
Follow directions
YES
NO
Move to a safer area to avoid more stings
Remove stinger as quickly as possible by scraping
with edge of fingernail or credit card
Remove any tight fitting jewelry from affected area
Wash area with soap and water
Apply ice or cold pack wrapped in cloth/towel for
10-15 minutes
Observe for at least 20 minutes or
Call EMS 9-1-1 if person’s symptoms worsen
Any signs of allergic reaction?
Is bite thought to be poisonous?
If an old bite, is it reddened, weeping,
ulcerated or sore?
NO
YES
Return to class, ensure adult supervisor aware
of bite and possible delayed allergic reaction.
If known history of anaphylaxis to insect
bite or envenomation and symptoms
are present, even if mild, administer
doctor and parent/guardian approved
medication.
Use EpiPen if prescribed.
YES
CALL 9-1-1
Contact
responsible school
nurse or
administrator &
parent/legal
guardian.
Emergency First Aid Guidelines for California Schools 22
Injury from a marine spine
requires evaluation for potential
foreign body and pain control
CALL EMS 9-1-1
See “Allergic
Reactions” (pg. 17)
Marine envenomation from bite, spine or
contact can cause anaphylaxis.
See “Allergic Reaction (pg. 17)
Marine field trips should carry first aid
kits with specific items for marine stings.
When unsure of marine animal or plant
contacted, obtain description and
Call POISON CONTROL CENTER
1-800-222-1222
Follow directions
Adult supervising person should be aware of sting and should
observe for allergic reaction.
Does person have:
Difficulty breathing? Hoarseness or difficulty swallowing?
Swelling of the face, throat or mouth?
A history of allergy to marine stings?
Fish bite
There will be pain
at the site; possible
breathing
difficulties
YES
NO
BITES & STINGS (MARINE)
Known history of
allergic reactions
should be recorded at
school and available
to all school staff. An
emergency care plan
is needed.
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
Sponge:
May leave tiny
spicules in skin
Spine Puncture: .
Stingray, Stonefish,
Sea Urchin or Star
fish - Causes
severe intense pain
Jellyfish
May cause severe
pain and shock
depending on
species
Coral
Rinse with sea
water or vinegar
to detoxify
Remove
spicules with
tape, rubber
cement or facial
mask
Immerse hand
or foot in hot
(not scalding)
water for 30-90
minutes to
relieve pain
Rinse with sea
water (not fresh)
Apply vinegar,
rubbing alcohol,
baking soda, if
available
Remove
adherent
nematocysts by
applying shave
cream, baking
soda or talc and
scrape with razor
or sharp edge
Use hot fluid
Treat as wound
See “Wounds
(Puncture)” (pg.
72)
Apply pressure if
bleeding, clean
wound, apply
clean dry
dressing

Emergency First Aid Guidelines for California Schools 23
Immobilize the bitten extremity at or below the level of the heart
If at school, make person sit or lie down, keep at complete rest, avoid activity
(walking)
Keep victim warm and calm
Remove any restrictive clothing, rings, and watches
Wash with soap and water
Cover with clean compress
Monitor pulse, color and respirations; prepare to perform
CPR if needed
If greater than 30 minutes from emergency department:
Apply a tight bandage around the entire extremity where
the bite occurred. Do not cut off blood flow
Parents may transport for medical evaluation if condition
is not life threatening
If capable and off-road, walk slowly to road or trailhead
and then take to emergency department
CALL EMS 9-1-1
Is snake known as poisonous?
Is person not breathing? See “CPR (pg. 29)
BITES & STINGS (SNAKE)
Treat all snakebites as poisonous unless
snake is positively identified as harmless.
DO NOT cut wound
DO NOT apply tourniquet
DO NOT apply ice
ALL SNAKE BITES
Need medical evaluation.
Do not try to capture or kill snake.
Take picture, if possible, of snake.
If snake is dead send with victim
to hospital.
YES
NO or UNKNOWN
Contact responsible
school nurse or
administrator & parent or
legal guardian.
ENCOURAGE
MEDICAL CARE
Signs & Symptoms of Poisonous Bite:
Severe:
Fang marks or mark
Swelling of tongue or throat
Swelling, discoloration or pain at site
Rapid swelling and numbness
Rapid pulse, weakness, sweating, fever
Severe pain
Shortness of breath
Shock
Burning, numbness or tingling sensation
Pinpoint pupils
Blurred vision, dizziness, fainting
Twitching, seizures
Nausea & vomiting
Paralysis and unconsciousness
Loss of muscle coordination

Emergency First Aid Guidelines for California Schools 24
BLEEDING
CALL EMS 9-1-1
Bandage wound firmly, but not tight enough to compromise circulation
Check skin circulation frequently by checking for warmth, pinkness, and good sensation
If bandage is saturated with blood, Do Not remove it
Reinforce with another dressing over existing dressing/bandage, and
Hold firm pressure for 10 minutes
CALL EMS 9-1-1
Maintain Direct Pressure on wound.
Have person lie down
Elevate feet 8-10 inches, unless this
causes pain/discomfort, OR a
neck/back/hip injury is suspected
Keep person warm but not hot
Reinforce existing dressing and apply
pressure to wound as needed
Wear disposable gloves when exposed to blood or other
body fluids. Do not remove impaled object.
Is injured part amputated (severed)?
Is blood bright red or spurting?
Is muscle, fat or bone showing?
Is there continued uncontrollable
bleeding?
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
Wash surrounding area with soap
and water
Rinse, pat dry, and apply bandage
If deep or gaping, wounds may
need stitches –
RECOMMEND MEDICAL CARE
Press firmly with a clean gloved hand, cloth or dressing for several minutes to
stop bleeding
Object in wound, see “Wound-Puncture” (pg. 72)
Elevate bleeding extremity. If fracture is suspected, see “Fractures…” (pg. 47)
If amputated part, place part in sealed plastic bag and place bag in ice
water
DO NOT PUT AMPUTATED PART DIRECTLY ON ICE
Send part in bag to the hospital with person
NO
YES
YES
NO
Emergency First Aid Guidelines for California Schools 25
Wash area with soap and water
DO NOT BREAK BLISTER
If ruptured blister, clean and cover with “2
nd
skin bandage,”
plain athletic tape, or “mole skin” type bandage
If intact blister, apply dressing and avoid further friction
(different shoes, if possible)
If red, sensitive but no blisters, apply tape directly over area
Apply bandage, tape or dressing to prevent further rubbing
Wear disposable gloves when exposed to blood and other body
fluids.
If infection is
suspected,
contact responsible
school nurse or
administrator &
parent or legal
guardian.
BLISTERS (FROM FRICTION)
Blisters heal best when kept clean and dry with
avoidance of further friction at blister site.

Emergency First Aid Guidelines for California Schools 26
BRUISES
Rest injured part
Apply cold compress or ice bag
covered with a cloth or towel, to
injured part (not more than 20 min)
If a child comes to school
with unexplained,
unusual or frequent
bruising, consider the
possibility of child abuse.
See
"Child Abuse" (pg. 35)
Is there rapid swelling?
Is person in great pain?
If it is too
uncomfortable to
return to normal
activities, contact
responsible school
nurse or
administrator &
parent or legal
guardian.
Consider other potential injuries
and see appropriate guide.
Contact responsible school
authority & parent or legal
guardian.
ENCOURAGE IMMEDIATE
MEDICAL CARE OR
CALL EMS 9-1-1
A bruise is bleeding under the skin. Bleeding is usually
self-limited by pressure of surrounding tissues. Initially
red, later turning dark colors like purple. An old bruise
later may turn yellow then green.
Painful, large bruises or marked swelling areas may
indicate more severe damage of muscle, bone, or
internal tissues that need medical care.
If skin is broken:
Treat as a cut.
See "Wounds" (pg. 71)
If fracture suspected,
See “Fractures…” (pg. 47)
YES
NO

Emergency First Aid Guidelines for California Schools 27
CHEMICAL OR HEAT
(THERMAL)
ELECTRICAL
What type of burn is it?
Always make sure that the situation is safe
for you before helping the person.
Burns may be associated with other injuries,
see appropriate topic.
BURNS
Are any of these findings present:
Confused or unconsciousness?
Difficulty breathing?
Soot around mouth or nose?
Burn on face or eye?
Burn is deep or includes a large area, or multiple
parts of the body?
Burned skin is white, brown, black or charred?
Burn is from an explosion?
Are there other injuries?
Remove from source of burn
Maintain airway and breathing, see “CPR” if needed (pg. 32)
CALL EMS 9-1-1
Turn off electrical power
Check for breathing and other injuries
Cover with a dry, preferably sterile, clean dressing
Maintain normal body temperature
Electric shock that leaves a visible burn
requires medical attention
See “Electric Shock”
NO
YES
See “Burns
Thermal and
Chemical”
(pg. 28)
Emergency First Aid Guidelines for California Schools 28
Heat (Thermal) Chemical
Cover with dry dressing
For burns on multiple parts
of body cover with dry clean
sheet. Keep air off burn
DO NOT USE ointment on
burns unless directed by a
physician
Wear gloves and, if possible, goggles
Avoid chemical contact
Brush off dry chemicals from skin
Remove all clothing and jewelry possibly
exposed to chemical
Rinse chemicals off skin, eyes and away
from body IMMEDIATELY with large
amounts of water. Rinse for 10 minutes.
If eyes are involved, see “Eyes” (pg. 42)
Try to identify substance
CALL POISON
CONTROL CENTER
1-800-222-1222
while flushing burn & ask for
instructions.
Follow directions received.
Contact responsible
school nurse or
administrator & parent
or legal guardian, if
more than a small
superficial burn.
ENCOURAGE
URGENT MEDICAL
CARE
If person comes to
school with patterned
burns (e.g., iron or
cigarette shape) or glove-
like burns, consider the
possibility of abuse.
See "Child Abuse” (pg.
35)
BURNS (CONT.)
What type of burn is it?
Flush all burns with cool
running water
Cover large burns with a
clean dry cloth
Cover smaller burns loosely
with a clean, cool, damp
cloth to cool the burn and
relieve pain
Keep victim warm
DO NOT BREAK BLISTERS
Keep wound/burn clean
Treat other injuries
Persons with small and
superficial burns (e.g.,
sunburn without blisters)
may return to class unless
so uncomfortable they are
unable to participate
Check person's immunization record for DT, DPT
(tetanus). See "Tetanus" for more information.
Emergency First Aid Guidelines for California Schools 29
NOTES ON PERFORMING CPR
The American Red Cross (ARC) guidelines follow the American Heart
Association’s (AHA) new CPR guidelines for laypersons, “Guidelines 2010 for
Emergency Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.”
BARRIER DEVICES
Barrier devices, to prevent the spread of infections from one person to another,
can be used when performing rescue breathing. Several different types exist (e.g.,
face shields, pocket masks). It is important to practice using these devices in the
presence of a trained CPR instructor before attempting to use them in an
emergency situation.
AUTOMATED EXTERNAL DEFIBRILLATORS (AEDs)
AEDs are devices that help to restore a normal heart rhythm when the heart is
not beating properly. It does this by delivering an electric shock to the heart.
A physician’s prescription is required to purchase an AED. A physician is also
required to provide medical direction to the school or school district that acquires
an AED. If your school has an AED, obtain training in its use, and training in CPR,
before an emergency occurs. The majority of AED use in the schools will be on
adults at the facility, since the medical conditions likely to require use of an AED
on a child are extremely rare.
AED training is offered through the American Heart Association, the American Red
Cross, the American Health and Safety Institute, the National Safety Council and
other CPR and AED training programs. AED manufacturers also offer training.
The AED regulations are available at the EMS Authority’s website
http://www.emsa.ca.gov. See CA Code of Regulations, Title 22, Division 9,
Chapter 1.8, Training Standards and Utilization for Use of the Automated External
Defibrillator by Non-Licensed and Certified Personnel for further information.
CPR

Emergency First Aid Guidelines for California Schools 30
AUTOMATED EXTERNAL DEFIBRILLATORS (AED)
CHECK WHICH APPLIES:
NO AED AVAILABLE AT
THIS SCHOOL.
My School’s AED is
located at:
Persons must be trained to use an AED. After receiving training on
how to use the AED, remember to:
Check for unresponsiveness
Call 9-1-1 and retrieve the AED
Check for unresponsiveness or gasping breathing
If unresponsive or breathing only gasping begin chest
compressions
Turn on AED and follow directions
Attach AED electrode pads, analyze rhythm
When the AED recommends the patient needs to be shocked,
make sure no one is touching the person and press the “Shock”
button
Follow instructions from AED unit
If instructed to do so by AED, resume CPR for 2 minutes and follow
instructions from AED device
If no signs of circulation, resume CPR

Emergency First Aid Guidelines for California Schools 31
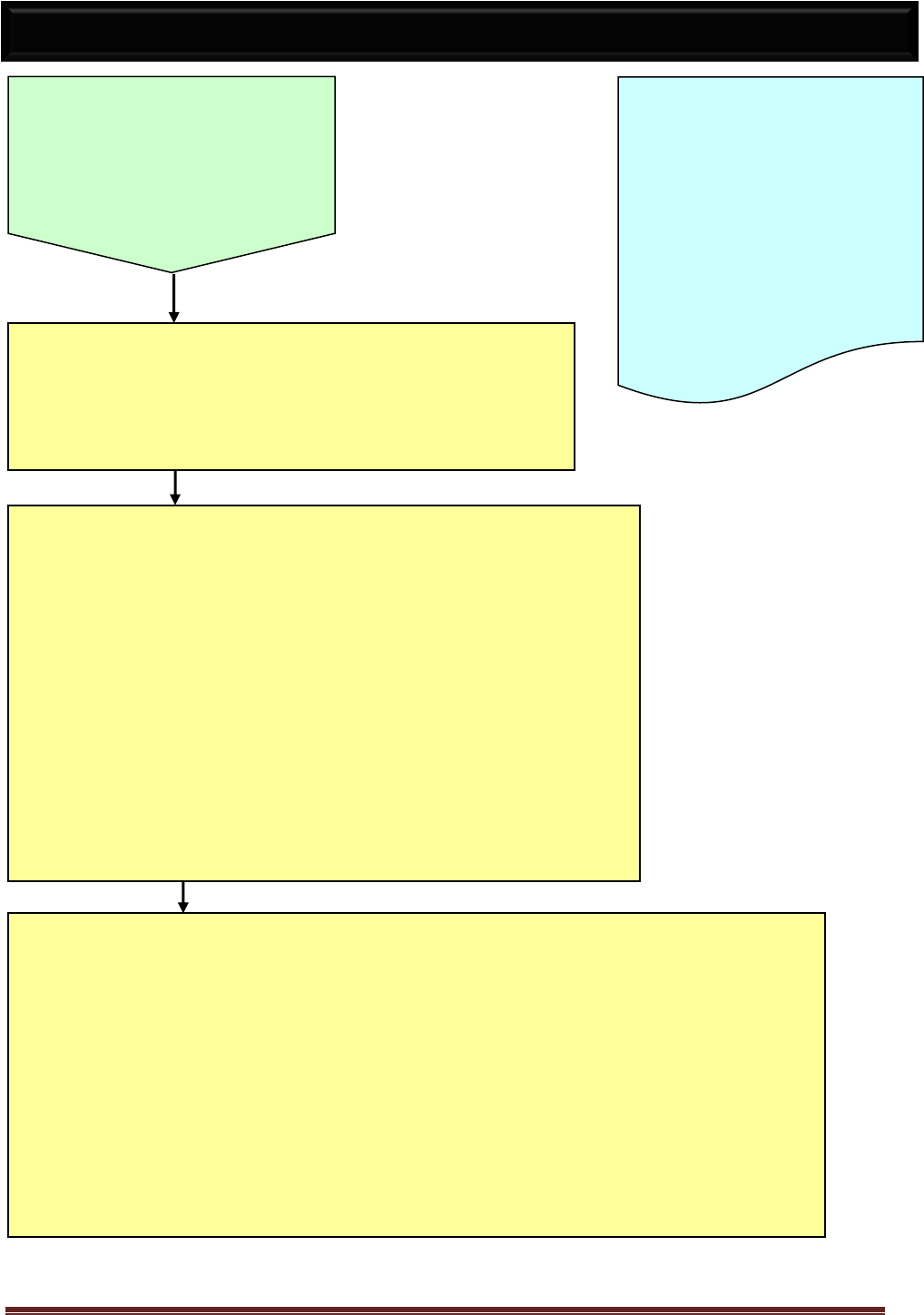
CHECK FOR
UNRESPONSIVENESS
(Call out, rub arms/chest).
If responsive, no CPR needed.
If unresponsive, call 9-1-1.
If anyone else available, have them call
for help and an AED.
BEGIN CHEST COMPRESSIONS AT A RATE OF
100/MIN; deliver 30 compressions
Infants: use 2 fingers in middle of breast bone and
compress ½” -1” inch
Small children: use heel of hand, compress 1½”-2”
Adults: use both hands – one on top of other in
middle of breast bone and compress at least 2” –
allow for full recoil of chest
Place on left side
and protect airway
CALL 9-1-1
See “Loss of
Consciousness”
and provide first aid
as needed (pg. 53).
Additional written
directions and
pictures on next
page (pg. 32).
If
Breathing
If NOT
Breathing or only
Gasping
LAY PERSON CPR
If trained - Give 2 rescue breaths
Tilt head back and open jaw
Cover mouth with your mouth
Give breaths until chest rises
Continue with 30 compressions and 2
breaths
If untrained – continue “Hands only”
Continue breathing and chest compressions
as needed
REASSESS EVERY 2 MINUTES for
responsiveness; if unresponsive, continue
CPR
If patient starts breathing, place on left side
and protect airway
Adult CPR
Child CPR
Infant CPR
Head Tilt
Emergency First Aid Guidelines for California Schools 32
CPR is to be used when a child or adult is unresponsive or when breathing or heart beat stops.
1. Tap or gently shake the shoulder. Shout “Are you OK?” If that person is unresponsive,
shout for help and send someone to call EMS 9-1-1.
2. Turn the person onto his/her back as a unit by supporting the head and neck. If head
or neck injury is suspected, DO NOT BEND OR TURN NECK.
3. Lift chin up and out with one hand while pushing down on the forehead with the other
to open the AIRWAY. If head or neck injury suspected, hold head still and move jaw
forward to open airway.
4. Check for normal breathing by observation of chest, if there is no breathing or the patient is making gasping
breaths then begin chest compressions at a rate of 100 per minute. Compress 30 times before beginning
rescue breaths.
5. If child is not breathing, seal your lips tightly around his/her mouth; pinch nose shut.
While keeping the airway open, give 2 slow breaths (1 to 1½ seconds per breath) until chest rises.
IF AIR GOES IN:
(Chest rises with rescue breath)
6. Place heel of one hand on the lower half of
breastbone. Do NOT place your hand over the
very bottom of the breastbone.
7. Compress chest 30 times with heel of one hand
(at least 2 inches). Lift fingers to avoid pressure
on ribs.
8. Give 2 slow breaths until chest rises.
9. REPEAT CYCLES OF 30 COMPRESSIONS TO 2
BREATHS AT A RATE OF 100 COMPRESSIONS
PER MINUTE UNTIL PERSON SHOWS SIGNS
OF BREATHING EFFECTIVELY ON OWN,
SHOWS OTHER SIGNS OF CIRCULATION, OR
HELP ARRIVES.
IF AIR WON’T GO IN:
(Chest does NOT rise with rescue breath)
6. Re-tilt head back (Steps 3-5). Try to give 2 breaths
again.
IF AIR GOES IN, FOLLOW LEFT COLUMN.
IF AIR STILL WON’T GO IN:
7. Find hand position near center of
breastbone. Do NOT place your hand
over the very bottom of the breastbone.
8. Compress chest 30 times with the heel of 1 hand (at
least 2 inches). Lift fingers to avoid pressure on ribs.
9. Lift jaw and tongue and look in mouth. If foreign
object is seen, sweep it out with finger. If object is not
seen, Do Not Sweep With Finger Blindly.
10. REPEAT STEPS 6-9 UNTIL BREATHS GO IN,
CHILD STARTS TO BREATH EFFECTIVELY ON
OWN, SHOWS OTHER SIGNS OF CIRCULATION
OR HELP ARRIVES.
1. Reproduced with permission, Pediatric Basic Life Support ©
1997, Copyright American Heart Association
2. Text based on Community First Aid & Safety, 2002 American
Red Cross
3. 2010 American Heart Association Guidelines for CPR
LAY PERSON CPR
(CON’T)
FOR CHILDREN ONE YEAR OLD TO ADULT

Emergency First Aid Guidelines for California Schools 33
CHOKING
FOR CONSCIOUS VICTIMS
Call 9-1-1 or activate EMS after starting rescue efforts.
INFANTS UNDER ONE YEAR OF AGE
Begin the following if the infant is choking and is unable to
breathe. However, if the infant is coughing or crying, DO
NOT do any of the following, but call EMS 9-1-1, try to
calm the child and watch for worsening of symptoms. If
cough becomes ineffective (loss of sound), begin step 1
below.
1. Position the infant, with head
slightly lower than chest, face
down on your arm and support the
head (support jaw; do NOT
compress throat).
2. Give up to 5 back blows with the
heel of the hand between infant’s shoulder blades.
3. If object is not coughed up,
position infant face up on your
forearm with head slightly lower
than rest of body.
4. With 2 or 3 fingers, give up to 5
chest thrusts near center of breastbone, about one
finger width below the nipple
line.
5. Open mouth and look. If foreign
object is seen sweep it out with
finger.
6. Tilt head back and lift chin up
and out to open the airway. Try
to give 2 breaths.
7. Repeat steps 1-6 until object is coughed up, infant
starts to breathe or infant becomes unconscious.
IF INFANT BECOMES UNCONSCIOUS, LAY ON
BACK AND GO TO PAGE 32, RIGHT COLUMN,
STEP 6 OF CPR INSTRUCTIONS USING 2
FINGERS IN MIDDLE OF BREAST BONE FOR
COMPRESSIONS.
CHILDREN OVER ONE YEAR OF AGE & ADULTS
Begin the following if the child/adult is choking and is
unable to breathe. However, if the child/adult is coughing
or crying, DO NOT do any of the following, but call EMS 9-
1-1, try to calm the child/adult and watch for worsening of
symptoms. If cough becomes ineffective (loss of sound),
begin step 1.
1. Stand or kneel behind person and place your arms
under the armpits to encircle the chest.
2. Place thumb side of fist against
middle of abdomen just above
the navel. DO NOT place your
hand over the very bottom of
the breastbone. Grasp fist
with other hand. Press with
quick backward and upward
thrusts.
3. Give up to 5 quick inward and upward thrusts.
4. Repeat steps 1-2 until object is coughed up, or person
starts to breathe or becomes unconscious.
IF PERSON BECOMES UNCONSCIOUS, LAY ON
BACK AND GO TO PAGE 32, RIGHT COLUMN,
STEP 6 OF CPR INSTRUCTIONS.
FOR OBESE OR PREGNANT PERSON
Stand behind person and place your arms under the
armpits to encircle the chest. Place thumb side of fist
against lower half of breastbone and thrust backwards.
1. Reproduced with permission, Pediatric Basic Life Support,
© 1997, Copyright American Heart Association
2. Text based on Community First Aid & Safety, 2002 ,
American Red Cross

Emergency First Aid Guidelines for California Schools Page 34
Signs & Symptoms Of A Heart Attack
Chest pain described as constant heavy pressure, vise like, or pain in the middle or upper
chest. The discomfort may travel across the chest to arm, neck or jaw and also include:
o Left arm/shoulder pain
o Jaw/neck pain
o Sudden unexplained weakness or dizziness with or without nausea
o Sweaty, clammy, pale, ashen or bluish skin
o Shortness of breath or breathing is abnormal
CHEST PAIN (POSSIBLE HEART ATTACK)
If unconscious, see “Loss of
Consciousness” (pg. 53)
If breathing stops; see “CPR” (pg. 32)
Place in position of comfort
Keep calm, don’t panic, reassure person
DO NOT GIVE MEDICATIONS UNLESS
AUTHORIZED
CALL EMS 9-1-1
Even if person objects.
Do not transport by private car.
Cardiovascular disease and heart
attacks are rare among children
under 18 years of age. However,
some children have a history of heart
problems. Check emergency
medical information.
The risk of heart attack increases
steadily over 40 years of age.
Any loss of consciousness or confusion?
Does person look seriously ill?
Has heart attack symptom(s)? (see below)
Has significant chest pain stopped and returned?
Contact responsible
school nurse or
administrator &
parent/legal
guardian.
Ask person if this has
occurred before and
what made it better
Place in position of
comfort, usually
reclining, and keep quiet
Loosen tight clothing
Chest pain can be caused by:
Injury
Esophageal spasm
Lung inflammation
Pneumonia
Gastric disturbance
Anxiety/Stress
Heart conditions
YES
NO
Emergency First Aid Guidelines for California Schools Page 35
CHILD ABUSE & NEGLECT
Child abuse is a
complicated issue with
many potential signs.
Anyone in a position to
care for children should
be trained in recognition
of child abuse/neglect.
Mandated reporters
should receive required
annual training.
Teachers and other professional school staff are
required to report suspected abuse and neglect to the
Child Protective Services Agency. Refer to your own
school's policy for additional guidance on reporting.
Child Protective Services # _____________
Abuse may be physical, sexual or emotional in
nature. This is NOT a complete list:
Depression, hostility, low self-esteem, poor self-image
Evidence of repeated injuries or unusual injuries
Lack of explanation or unlikely explanation for an injury
Pattern bruises or marks (e.g., burns in the shape of a
cigarette or iron, bruises or welts in the shape of a hand)
"Glove-like" or "sock-like" burns on hands or feet
Unusual knowledge of sex, inappropriate touching or
engaging in sexual play with other children
Poor hygiene, underfed appearance
Severe injury or illness without medical care
If a child reveals abuse to you:
Stay calm
Take the child seriously
Tell the child that he/she did the right thing by telling you
Do not make promises that you cannot keep
Respect the sensitive nature of the child's situation. Remember each case
is individual and use your best judgment to act in the best interest of the child
Follow appropriate reporting procedures
See Department of Social Services, Publication 132 “The California Child
Abuse & Neglect Reporting Law - Issues and Answers for Mandated
Reporters,” at http://www.dss.cahwnet.gov/pdf/PUB132.pdf
If child has visible injuries,
refer to the appropriate
guideline to provide first aid.
Call EMS 9-1-1 if any injuries
require immediate medical
care.

Emergency First Aid Guidelines for California Schools Page 36
COMMUNICABLE DISEASES
A communicable disease
is a disease that can be
spread from one person
to another. Germs cause
communicable diseases
(bacteria, virus, fungus,
parasites).
For more information on protecting yourself from upper
respiratory infections listed under the "Emergency
Procedures" tab, see "Infection Control" (pg. 16).
In general, there will be little that you can do for a person in school who has an infection; however, limit
the exposure and spread of disease to others by encouraging student(s) to cover mouth and nose when
coughing or sneezing; use a tissue and encourage hand washing or use of alcohol based hand gel.
Refer to your school's exclusion policy for illness.
Common diseases include: Chicken pox, head lice, pink eye, strep throat and
influenza (flu).
Does the person have
SIGNS OF LIFE-THREATENING ILLNESS:
Difficulty breathing or swallowing, rapid breathing?
Severe coughing, noisy breathing?
Fever over 100.0 degrees F in combination with lethargy,
extreme sleepiness, abnormal behavior
Does the person have?
SIGNS OF PROBABLE ILLNESS or INFECTION:
Redness, swelling, drainage of eye?
Unusual spots/rash with fever or itching?
Crusty, bright yellow, swollen, tender, red or open
draining skin sores?
Diarrhea (more than two loose stools a day)?
Vomiting?
Yellow skin or yellow "white of eye"?
Fever greater than 100.0 degrees F?
Extreme tiredness or lethargy?
Unusual behavior?
Additional signs & symptoms:
Fussiness
Runny nose
Mild cough
Headache
Itchy scalp
Stomach ache
Sore throat
Ear ache
Remove student
from the
classroom, contact
responsible school
nurse or
administrator and
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
Monitor child for
worsening of
symptoms and
contact parent/legal
guardian.
CALL EMS 9-1-1
YES
NO
YES

Emergency First Aid Guidelines for California Schools Page 37
DIABETES
A person having a diabetic reaction could have the
following signs & symptoms:
Irritability and upset
Rapid pulse
Sweating and feeling “shaky”
Cramping
Change in behavior
Dizziness
Unconsciousness
Listlessness
Rapid, deep breathing
Pallor
Seizure
Confusion
Fruity or sweet breath
Give the person any one of the
following:
Fruit juice or soda pop (not diet) 6-
8 ounces
Sugar (2 packets or 2 teaspoons)
dissolved in water or juice
Cake decorating gel (1/2 tube) or
icing
Instant glucose gel
Continue to watch the person in a
quiet place
Is person improving?
CALL EMS 9-1-1
If unconscious, see “Loss of
Consciousness” (pg. 53)
A person with
diabetes should be
known to appropriate
school staff.
A history should be
obtained and an
emergency care plan
should be developed at
time of enrollment.
Is the person:
Unconscious?
Confused or acting unusual?
Having a seizure?
Unable to speak?
Having rapid, deep breathing?
Does he/she have a blood
sugar monitor available?
Does person have an
emergency action/care plan?
Contact
responsible school
nurse or
administrator &
parent or legal
guardian.
Allow person to check blood
sugar*
Follow Emergency Action/Care
Plan
NO
YES
NO
YES
YES
YES
NO
NO

Emergency First Aid Guidelines for California Schools Page 38
Wear disposable gloves when
exposed to blood or other body
fluids. A person may come to the
office because of repeated
diarrhea, or after an “accident” in
the bathroom.
DIARRHEA
Check temperature
Allow the person to rest if experiencing any stomach pain
Give the person small amounts of fluid (water, sport drink,
etc.) to drink to prevent dehydration; avoid sodas
Juice or sports drink mixed 50/50 with water
Contact responsible school nurse or administrator & parent or legal
guardian and urge medical care if:
Has three or more episodes of diarrhea
The person has a fever, over 100.0 degrees F, see “Fever” (pg. 45)
Blood is present in the stool
The person is dizzy and pale
The person has severe stomach pain
If the person’s clothing is soiled:
Maintain privacy, offer change of clothing or
a blanket to wrap up in
Wear disposable gloves
Double-bag the clothing to be sent home
Wash hands
thoroughly

Emergency First Aid Guidelines for California Schools Page 39
DROWNING/NEAR DROWNING
Give rescue breaths, if not
breathing, see “CPR”
(pg. 32)
CALL EMS 9-1-1
DO NOT MOVE VICTIM
Contact responsible school
authority and parent/legal
guardian.
Monitor breathing, level
of consciousness and
circulation
If changes occur, see
appropriate guideline
See appropriate
guidelines
Drowning can occur
in 2 inches of liquid.
Immediate medical
care is needed.
CPR trained staff should send someone for help.
Get person out of the water.
Place on back with head and neck straight.
Open and maintain AIRWAY (if head or neck injury
suspected or unknown, assume injury and lift jaw
without moving head).
Assess breathing.
Clear airway of vomit/objects if needed.
Support head & neck and turn body and head as
one (logroll) to the left side.
Minimize head & neck movement.
Support head, keep airway open
Is victim:
Not breathing?
Unconscious, confused, lethargic?
Was victim injured?
Contact responsible
school nurse or
administrator & parent or
legal guardian.
ENCOURAGE
IMMEDIATE MEDICAL
CARE
Is patient regurgitating water?
?
If victim recovers with initial
rescue efforts, complications
may still occur after near
drowning.
YES
YES
YES
NO
Support head & neck & turn body & head
as one (logroll) to the left side
Minimize head & neck movement
NO
NO

Emergency First Aid Guidelines for California Schools Page 40
OBJECT IN EAR CANAL
EARS
Gently tilt head.
Take & record
temperature
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL
CARE
Ask person if he/she
knows what is in the ear
Is there a live insect
in the ear?
Put drop of oil in
ear. Did object
come out?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
DO NOT ATTEMPT
TO REMOVE INSECT
OR OBJECT
Do Not use a light to
attract an insect out, it
may excite the insect.
DRAINAGE FROM EAR or EARACHE
DO NOT:
Try to clean out ear
Plug ear canal
Stop flow of drainage
YES
NO
YES
NO or NOT SURE

Emergency First Aid Guidelines for California Schools Page 41
ELECTRICAL INJURY
Send someone to
CALL EMS 9-1-1
Did person lose
consciousness or become
unresponsive?
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
Contact responsible
school nurse or
administrator &
parent or legal
guardian, if injured.
ENCOURAGE
URGENT
MEDICAL CARE
If patient is
unresponsive and
no one else is
available to call
EMS, call EMS
yourself then
begin CPR.
If a person has signs of an electrical
burn, it may be subtle:
Check for other injuries
Apply clean, dry dressing
DO NOT use ointments
Protect from hot and cold
All electrical burns need medical
attention. Electrical current can
travel through the underlying
tissues and cause unseen injury
If unresponsive or has
only gasping breathing,
begin CPR;
see “CPR” (pg. 32)
Injury from any electric source other than
household, Call 9-1-1
If exposed power source, TURN OFF POWER
SOURCE, if possible
DO NOT TOUCH PERSON UNTIL POWER
SOURCE IS SHUT OFF
Once power is off and situation is safe, approach
the person and ask, “Are you okay?”
Any electrical shock with injury needs medical
evaluation
YES
NO

Emergency First Aid Guidelines for California Schools Page 42
EYES (INJURY)
Keep person from rubbing eye, or moving object.
DO NOT TOUCH THE EYE
OR
PUT ANY PRESSURE ON THE EYE OR THE OBJECT
CALL EMS 9-1-1
Keep person
comfortable with head
and chest in sitting
position or elevated and
quiet.
Is injury severe?
Is there a change in vision?
Has object penetrated eye or eye socket?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
IMMEDIATE
MEDICAL CARE
.
Contact
responsible school
nurse or
administrator &
parent or legal
guardian.
If an object has penetrated the eye
or eye socket,
DO NOT REMOVE OBJECT.
A large object should be
supported with dressings to
minimize movement.
EYES CONTINUED ON
NEXT PAGE (pg. 43)
With any eye problem, ask if
the person wears contact
lenses. Have person
remove contacts before
giving any first-aid to eye.
YES
NO

Emergency First Aid Guidelines for California Schools Page 43
EYES (CONT.)
Have person blink repeatedly to flush out particle
If necessary, lay person down, & tip head toward
affected side
Gently pour cool tap water over open eye to
flush out particle
Immediately flush eye with large amounts of tepid or cool, clean water
Tip the head so that the affected eye is below the unaffected eye
washing the eye from nose to side of face for 5-10 minutes
While flushing eye try to determine substance that entered eye and
Call POISON CONTROL CENTER
1-800-222-1222
Follow Instructions
Follow Instructions.
If eye has been injured by a chemical
or continued pain or visual change
CALL EMS 9-1-1
If particle does not flush
out of eye, or if eye pain
continues, contact
responsible school nurse
or administrator and
parent or legal guardian.
ENCOURAGE MEDICAL
CARE
Close Eyelid & Cover
Wear gloves and if
possible, goggles.
Ask what is in eye?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
PARTICLE IN EYE:
Keep person from
rubbing eye.
Ask what is in eye?
CHEMICALS IN EYE

Emergency First Aid Guidelines for California Schools Page 44
FAINTING
See appropriate guideline.
If head or neck injury
suspected. Treat as
possible neck injury.
See “Neck & Back Pain”
(pg. 56).
DO NOT MOVE PERSON
Keep person in flat position lying on back
Elevate feet above level of heart
Loosen clothing around neck and waist
If you observe, or the person complains of any of
the following signs or symptoms of fainting, have
the person lie down to prevent injury from falling:
Extreme weakness or fatigue
Dizziness or light-headedness
Extreme sleepiness
Pale, sweaty skin
Nausea
Fainting may have many causes
including: injuries, blood loss,
poisoning, severe allergy, diabetic
reaction, heat exhaustion,
hypoglycemia, illness, fatigue,
stress, not eating, standing still for
too long, etc.
Most persons who faint will recover
quickly when lying down. If person
does not regain consciousness within
1 minute, see “Loss of Consciousness”
(pg. 53) and CALL 9-1-1.
Did person injure self when he/she
fainted/fell?
Are symptoms (dizziness,
light-headedness, weakness,
fatigue, etc.) still present?
Contact
responsible
school nurse or
administrator &
parent/legal
guardian.
Keep airway clear and monitor breathing
Keep person warm, but not hot
Control bleeding if needed , see “Bleeding” (pg. 24)
Give nothing to eat or drink
Check for a medical alert tag or bracelet
If person feels
better, and there
is no danger of
neck injury,
he/she may be
moved to a
quiet, private
area.
Is fainting due to a forceful injury?
CALL EMS 9-1-1
See “Loss of
Consciousness” (pg. 53).
NO
NO
YES or NOT SURE
YES
NO
YES
YES
Keep person lying down.
Contact responsible school
nurse or administrator &
parent or legal guardian.
ENCOURAGE URGENT
MEDICAL CARE

Emergency First Aid Guidelines for California Schools Page 45
If alert, give fluids (i.e., juices, water,
soup or gelatin) as tolerated
Avoid overheating with excessive
clothing/blankets
Take person’s temperature, if possible.
Note temperature over 100.0 degrees F as
fever.
Have the person lie down in a room that affords privacy.
Give no medications unless previously authorized; such
as acetaminophen or ibuprofen
Contact
responsible
school nurse
or
administrator
& parent or
legal
guardian.
CALL EMS 9-1-1
Is Temp over
100.0 degrees F?
Does child have fever and
Is unresponsive?
Is limp, weak, listless or not moving?
Rash with purple spots?
Limited movement of neck (stiff)?
First time seizure? See “Seizures” (pg.62)
Severe headache?
Abdominal pain?
Difficulty breathing?
FEVER & NOT FEELING WELL
YES
YES
NO
NO

Emergency First Aid Guidelines for California Schools Page 46
If you suspect a
fracture, see
“Fractures…” (pg. 47).
Wear gloves if bleeding
Use gentle direct pressure until bleeding stops.
Wash with soap and water, apply Band-Aid or tape
overlay to protect nail bed
Apply ICE PACK for 10-20 minutes for pain and
prevent swelling
Return to class
Assess history of injury and examine injury.
A crush injury to fingertip may result in fracture or
bleeding under intact fingernail, creating pressure
that may be very painful.
After 20 minutes of ICE, has pain subsided?
Can student grasp or pinch without significant
pain?
Contact
responsible
school nurse or
administrator &
parent/legal
guardian.
Contact
responsible school
nurse or
administrator &
parent/legal
guardian.
ENCOURAGE
MEDICAL CARE
FINGERNAIL/TOENAIL INJURY
YES
NO

Emergency First Aid Guidelines for California Schools Page 47
CALL EMS 9-1-1
Avoid movement of injured part
Do not allow person to put weight on it or use it
Splint with towel, cardboard, or sling
Gently support and elevate injured part and adjacent
joint, with pillow or folded towel, if possible
Apply ice/cold (no more than 20 min/hr.), covered with
cloth or paper towel
Is bone or joint deformed or bent in an unusual
way?
Is skin broken over possible fracture?
Is bone sticking through skin?
Is skin of the injured extremity pale/cool when
compared with opposite extremity?
Is there loss of feeling or movement?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
If discomfort
is gone,
allow person
to return to
class.
After a period of rest, recheck the injury.
Is the pain gone?
Can person move or put weight on injured part without
discomfort?
Is numbness/tingling gone?
Has normal sensation returned to injured area?
Is coloration, circulation normal?
If bleeding, wear gloves and apply
direct pressure to bleeding site.
Control Bleeding, see “Bleeding”
(pg. 24)
Leave in position of comfort
Cover broken skin with clean
bandage
Do NOT move or attempt to
straighten injured part
Splint
Give nothing to eat or drink
See “Seriously Ill/Shock” if needed
(pg. 63)
Signs & Symptoms of Fracture, Dislocation, Sprains or Strains
Pain and/or swelling in one area
Cold and numb
Large bruise/discoloration
Loss of sensation or movement
Sounds/feels like bones moving
rubbing
Disfigurement at joint
Bent or deformed
bone/extremity
FRACTURES, DISLOCATIONS, SPRAINS OR STRAINS
Treat all injured parts as if they
Could be fractured (See Signs &
Symptoms at bottom of page)
YES
NO
NO
YES
Contact responsible
school nurse or
administrator & parent
or legal guardian.
ENCOURAGE
MEDICAL
CARE

Emergency First Aid Guidelines for California Schools Page 48
YES
Take to warm place and remove cold or wet clothing and replace with warm, dry
clothes
Protect cold part from further injury (may not have any sensation)
Do NOT rub or massage the cold part OR apply heat such as a water bottle or hot
running water
Put affected body part in bath temperature water to warm & potentially thaw
Cover part loosely with nonstick, clean dressing or dry blanket
Keep person and part warm
CALL 9-1-1
Keep person and affected
area warm
Frostbite can result
in the same type of
tissue damage as a
burn. It is a serious
condition and
requires medical
attention.
Does extremity or body part:
Look discolored – grayish, white or waxy?
Feel firm hard (frozen)?
Have a loss of sensation?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
NO
FROSTBITE
Exposure to cold even for short periods of time
may cause “Hypothermia” (a low temperature) in
children, see “Hypothermia” (pg. 52). The nose,
ears, chin, cheeks, fingers and toes are parts most
often affected by frostbite.
Frostbitten skin may:
Look discolored, grayish-yellow, pale, or
white)
Feel cold to touch
Feel numb to the person
Deeply frostbitten skin may:
Look white or waxy
Feel firm-hard (frozen)

Emergency First Aid Guidelines for California Schools Page 49
.
YES
Have person rest, lying flat
Keep person quiet & warm
Turn the head and body together to the
left side, keeping the head and neck in a
straight line with the trunk.
CALL EMS 9-1-1
Look, listen & feel for
breathing. If person stops
breathing,
see “CPR” (pg. 32)
GIVE NOTHING TO EAT
OR DRINK
Is person vomiting?
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
With a head injury (other than minor head
bump), always suspect neck injury as well.
Do NOT move or twist the spine or neck,
see “Neck & Back Pain” (pg. 56).
Watch person closely.
DO NOT LEAVE PERSON ALONE
Are any of the following present:
Unconsciousness, seizure or neck pain?
Blood is flowing freely from the head wound, see
“Bleeding” (pg. 24)?
o Maintain firm, direct pressure
Inability to respond to simple commands?
Blood or watery fluid from ears or nose?
Inability to move or feel arms or legs?
Person is sleepy, confused or asks repetitive
questions?
Taking blood thinners (e.g., Coumadin)
HEAD INJURIES
NO
YES
YES
NO
If person only bumped head and
does not have any other
complaints or symptoms,
See “Bruises” (pg. 26).
Ask questions about how injury
occurred.
Many head injuries that happen
at school are minor. Head
wounds may bleed easily and
form large bumps. Bumps to the
head may not be serious. Head
injuries from falls, sports, &
violence may be serious. If head
is bleeding,
see “Bleeding” (pg. 24).
If person was briefly confused and
seems fully recovered contact responsible
school nurse or administrator & parent or legal
guardian.
WATCH FOR DELAYED SYMPTOMS &
ENCOURAGE MEDICAL CARE.
Send home instructions for observing delayed
symptoms.

Emergency First Aid Guidelines for California Schools Page 50
Has a head injury occurred?
Apply cold cloth or compress to head
Offer food or juice if person hasn’t eaten adequately
Allow to rest in quiet, low light room
Is temperature over
100.0 degrees F?
Is headache severe?
Are other signs or symptoms present?
(nausea, vomiting, fever, vision disturbance or
dizziness)
History of chronic headache, stiff neck, or
sensitivity to light (light hurts eyes)?
Is patient not alert or not thinking clearly
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
Give medication only if
previously authorized.
See “Fever”
(pg. 45)
HEADACHE
YES
YES
NO
NO
Have person lie down for a
short time in a room that
affords privacy. Headache
can be due to the lack of
adequate food or water.
Ask person when and what
they ate last.
See
“Head Injuries”
(pg. 49)
If not alert & in abnormal
mental state call 9-1-1.
YES
NO
If headache
persists, contact
responsible school
nurse or
administrator &
parent or legal
guardian.

Emergency First Aid Guidelines for California Schools Page 51
Give clear fluids frequently (water, sport
drink, etc.), in small amounts, if fully
awake and alert
If condition improves, may return to
class. NO P.E./Sports
If no improvement, child NEEDS
IMMEDIATE MEDICAL CARE
Quickly remove person from heat to
a cooler place
Put on side to protect airway
Look, listen and feel for breathing. If
not breathing, see “CPR” (pg. 32)
Remove outer clothing, as
appropriate. Cool rapidly by
completely wetting
clothing/skin with room
temperature water.
DO NOT USE ICE WATER.
CALL EMS 9-1-1
Move person to a cooler place
Have person lie down
Elevate feet
Loosen or remove outer clothing
Spray with water and fan person
Heat exhaustion is common and is due to lack of body
fluids. Heat Stroke is life-threatening and occurs when
the body is overwhelmed by heat and cannot regulate
body temperature. Strenuous activity in the heat may
cause heat-related illness. See signs & symptoms of
heat emergencies below.
Is person unconscious or altered mental status?
Are any of the following happening:
Hot, dry, red skin?
Altered mental status?
Vomiting? Fever?
Confusion, dizziness?
Rapid shallow breathing?
Signs & Symptoms of Heat Related Injury
Heat Exhaustion Heat Stroke
Cool, moist, pale skin
Hot skin (usually dry)
Weakness & fatigue
High temperature
Sweating, headache
Rapid, weak pulse
Vomiting, nausea
Rapid, shallow breathing
Confusion, dizziness
Seizure
Muscle cramping
Loss of consciousness
HEAT EXHAUSTION/HEAT STROKE
Spending too much time
in the heat, especially with
exertion, may cause heat
emergencies.
Heat emergencies can be
life-threatening situations.
YES
NO
NO
YES
Contact
responsible school
nurse or
administrator &
parent or legal
guardian.

Emergency First Aid Guidelines for California Schools Page 52
.
Take person to a warm place
Remove cold or wet clothing and
wrap in a warm, dry blanket
Hypothermia can happen from
exposure to cold, wet, & windy
conditions [does not require freezing
temperatures] when the body is no
longer capable of warming itself.
Young children are particularly
susceptible to hypothermia. It can be a
life-threatening condition if left
untreated for too long.
Hypothermia can occur after
being outside in the cold or
in cold water.
Does person have:
Decreasing consciousness?
Slowed breathing?
Confused or slurred speech?
White, grayish or blue skin?
No feeling in part of body?
Continue to warm with blankets
Provide a warm environment
If fully awake and alert, offer
warm (NOT HOT) fluids
If frostbite, do not rub, see
“Frostbite” (pg. 48) and do
not break blisters.
CALL EMS 9-1-1
Give nothing to eat or drink
Continue to warm with blankets
If sleepy or losing consciousness, place on left
side and protect airway, see “Loss of
Consciousness” (pg. 53)
Look, listen and feel for breathing. If
breathing stops, see “CPR” (pg. 32)
Contact
responsible
school nurse
or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL
CARE
Signs & Symptoms of Hypothermia (COLD)
Confusion
Shivering
Clumsy
Lethargic
Blurry vision
Abnormal behavior
Slurred speech
Impaired judgment
Uncoordinated
Slow, irregular pulse
HYPOTHERMIA (EXPOSURE TO COLD)
NO
YES

Emergency First Aid Guidelines for California Schools Page 53
.
Position person on their back
Loosen clothing around neck and
waist
Elevate feet and keep warm
Control bleeding if present
Give nothing by mouth
Keep person lying down 10-15
minutes
Loss of consciousness may have many causes
including: injuries, blood loss, poisoning, severe allergic
reaction, diabetic reaction, heat exhaustion, illness,
fatigue, stress, not eating, etc. If you know the cause
of the unconsciousness, see the appropriate guideline.
Did person regain consciousness?
Is unconsciousness due to injury?
Is person
breathing?
Treat as having possible neck
injury. See “Neck & Back Pain”
DO NOT MOVE person,
unless a threat exists.
Immobilize neck
Open AIRWAY using jaw
thrust maneuver
If vomiting, turn to left side
and support head in neutral
position with a towel roll
LOSS OF CONSCIOUSNESS
If victim stops
breathing, or has
gasping respirations
begin “CPR”.
YES
NO
NO
YES
If not breathing or gasping for
breath
Begin “CPR”
CALL EMS 9-1-1
See
“Fainting”
(pg. 44) or
“Seizures”
(pg. 62
YES or NOT SURE

Emergency First Aid Guidelines for California Schools Page 54
SEVERE
YES
NO
These may provide relief:
Short period of quiet rest
Warm (not hot) heating pad over lower abdomen
(if allowed by the school district)
Mild or severe symptoms/cramping
Abnormal bleeding
Is it possible the person is pregnant?
[Note: negative history is not reliable]
Menstrual problems may present
with:
Abdominal pain, cramping
Abnormal menses
Abnormal bleeding
Provide for
privacy
Give no medications unless previously
authorized by parent/legal guardian
If bleeding, offer a feminine pad
CALL EMS 9-1-1
Encourage medical care if disabling cramps
occur
ENCOURAGE IMMEDIATE MEDICAL CARE,
if heavy vaginal bleeding occurs (greater than
5 pads/tampons per day or continued bleeding
for 7 or more days)
Does person have continuing severe abdominal pain?
MENSTRUAL PROBLEMS
See
“Pregnancy”
(pg. 59)
YES or
NOT SURE
MILD
NO
For mild cramps
recommend
walking or regular
activities.
Contact responsible
school nurse or
administrator &
parent or legal
guardian.

Emergency First Aid Guidelines for California Schools Page 55
Have teeth been injured?
YES
YES
YES
NO
NO
NO
If unconscious:
Protect neck by keeping straight
Protect airway by log rolling on to left
side to allow drainage of blood
Gently support jaw with hand
See “Teeth & Gums” (pg. 68) for any
tooth injury
Control bleeding with direct pressure
Wear disposable gloves
when exposed to blood or
other body fluids. Use direct
pressure to control bleeding.
See “Head Injuries” (pg.
49) or “Neck Injury…”
(pg. 56) if you suspect
an injury other than
mouth or jaw.
If tongue, lips, or cheek are
bleeding, apply direct pressure
with sterile gauze or clean cloth
Look for difficulty breathing
Place cold compress over the
area to minimize swelling
CALL EMS 9-1-1
See
“Teeth &
Gums”
(pg. 66)
Does person have:
Difficulty breathing?
Choking sensation?
Loss of consciousness?
Persistent bleeding?
MOUTH & JAW INJURIES
Has jaw been injured?
Is cut large, deep?
Contact responsible
school nurse or
administrator and parent or
legal guardian.
ENCOURAGE
IMMEDIATE MEDICAL
CARE
Signs of jaw fracture include:
Marked tenderness from outer edge of jaw
Teeth do not fit together normally
Cannot open jaw widely
Painful to clench teeth

Emergency First Aid Guidelines for California Schools Page 56
NO
YES
LYING DOWN
WALK-IN
Keep person quiet and warm
Hold head still until EMS takes over care by gently
placing a hand on each side of head, OR
Place rolled up towels/clothing on both sides of
head so it will not move
DO NOT MOVE PERSON unless there is
IMMEDIATE DANGER of further physical
harm.
If person MUST be moved, support head and
neck – keep head, neck and back from
bending.
.
Allow person to assume position of
comfort.
Keep head straight
ADVISE PERSON NOT TO MOVE
HEAD OR NECK.
Suspect a neck/back injury if pain results from:
Falls over 8 feet or falling on head
Being thrown from a moving vehicle
Sports
Violence
Being struck by a car or other fast moving object
Has an injury occurred?
Did person walk-in or was
person found lying down?
Symptoms of Possible Spinal Nerve Injury
Loss of sensation
Numbness or
Loss of movement
tingling of arms
Electric shock-like pains
or legs
CALL EMS 9-1-1
NECK & BACK PAIN
If person is so uncomfortable
that he/she is unable to
participate in normal
activities contact responsible
school nurse or administrator
& parent or legal guardian.
May need medical
evaluation.
A stiff or sore neck from
sleeping in a “funny” position
is different than neck pain
from a sudden injury. Non-
injured stiff necks may be
uncomfortable, but they are
usually not emergencies.
Symptoms of Nerve Injury
(see below) need medical
evaluation, even if they
resolve.
Contact
responsible school
nurse or
administrator &
parent or legal
guardian.

Emergency First Aid Guidelines for California Schools Page 57
NO
YES or NOT SURE
OBJECT in NOSE
NO
YES
BROKEN NOSE (swollen and/or deformed with nose bleed)
Is object:
Large?
Puncturing nose?
Deeply imbedded?
Brisk nose bleed?
Have person hold the clear
nostril closed while gently
blowing nose.
Did object come out on its own?
DO NOT ATTEMPT TO REMOVE
OBJECT.
See “ Wounds-Puncture” (pg. 72) if
object has punctured the nose.
If object cannot be
removed easily,
DO NOT ATTEMPT
TO REMOVE.
NOSE CONTINUED
ON NEXT PAGE
(pg. 58)
Care as in “Nosebleed” on next page. Contact responsible
school authority and parent/legal guardian.
ENCOURAGE MEDICAL CARE
NOSE
If there is no pain,
person may return
to normal activity.
Notify parent or
legal guardian.
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
Can you see an object in
nose or did person put
something in their nose?

Emergency First Aid Guidelines for California Schools Page 58
NOSEBLEED
YES
NO
Nosebleed may be caused by
injury, allergy, blowing or
picking nose, or dryness.
Wear disposable gloves when
exposed to blood or other body
fluids
Lean head forward while sitting; if need
to lie down, lie down on side.
Pinch nostrils together just below nasal
bones, maintaining constant pressure
for 10-15 minutes.
If continued bleeding after pressure or if
injury to nose, apply cold pack to nose
for 10-15 minutes and continue to pinch
for bleeding
Person may return to
normal activity. Avoid
strenuous activity for
the day to prevent
recurrence of bleeding.
Notify parent or legal
guardian.
Has bleeding stopped?
Contact
responsible school
nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
Encourage mouth breathing and discourage
nose blowing, repeated wiping or rubbing.
NOSE (CONT.)
DO NOT TILT HEAD BACK
If head is tilted back, person
may spit up blood from throat.
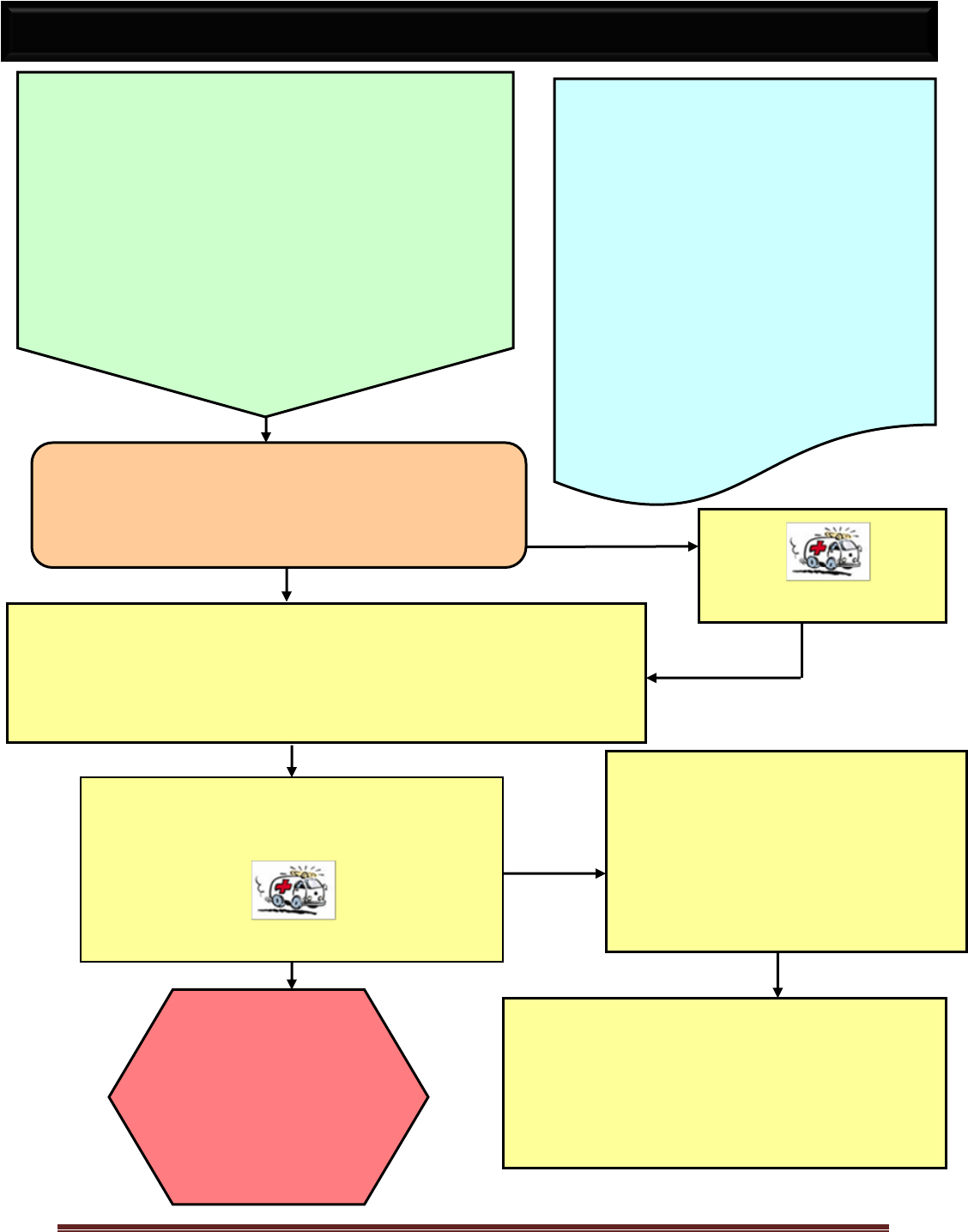
Emergency First Aid Guidelines for California Schools Page 59
YES
CALL POISON CONTROL CENTER
& follow instructions.
Phone # 1-800-222-1222
CALL EMS 9-1-1
.
Send sample of
vomited material,
or ingested
material with its
container (if
available), to the
hospital with the
person.
If person has any changes in level of
consciousness, place on his/her side and
look, listen and feel for breathing. If
breathing stops, see “CPR” (pg. 32)
Contact responsible school nurse or
administrator & parent or legal guardian
DO NOT INDUCE VOMITING or
give anything UNLESS Poison
Control instructs you to. With some
poisons, vomiting can cause greater
damage.
DO NOT follow the antidote label on
the container; it may be incorrect.
Wear gloves and remove any remaining substance in mouth.
If possible, find out:
Age and weight of person
What was swallowed or what type of “poison” it was
How much & when was it taken
Is person unconscious?
Is person having difficulty breathing? See “Loss
of Consciousness” (pg. 53)
CALL EMS 9-1-1
POISONING & OVERDOSE
Ask person if they ingested any medications or
other substances. Possible warning signs of
poisoning include:
Pills, berries or unknown substance in mouth
Burns around mouth or on skin
Strange odor on breath
Sweating, chest or abdominal pain
Upset stomach, vomiting, diarrhea
Dizziness or fainting
Seizure or convulsions
Remove source of poisoning or get person away
from toxic fumes.
Poisons can be swallowed, inhaled,
absorbed through the skin, eyes or
mucosa, or injected.
When you suspect poisoning:
CALL EMS 9-1-1 & Poison Control
Center: 1-800-222-1222
Continue to monitor
Airway
Breathing
Signs of circulation (pulse, skin
color, capillary refill)
Level of consciousness
Speech, orientation

Emergency First Aid Guidelines for California Schools Page 60
Vaginal Bleeding, if severe
CALL EMS 9-1-1
Severe Stomach Pain or Cramps
Person may be in labor or having a
miscarriage if cramps are strong and
repeat or “water has broken”
If labor suspected or if severe abdominal
pain persists
CALL EMS 9-1-1
Amniotic Fluid Leakage
This is NOT normal and may indicate the beginning of
labor or may lead to infection. Contact responsible
school nurse or administrator, and parent or legal
guardian.
Seizure
This may be a serious complication of late
pregnancy, see “Seizure” (pg. 62).
CALL EMS 9-1-1
For morning sickness,
see “Vomiting” (pg. 69).
Pregnancy may be
complicated by any of
the following:
PREGNANCY
Appropriate school staff should be
made aware of any pregnant
students. Ask if person might be
pregnant and when her last
menstrual period (LMP) occurred.
Keep in mind that any student who is
old enough to be pregnant might be
pregnant. NOTE: History may not
be reliable.
Contact responsible
school nurse or
administrator & parent or
legal guardian.
ENCOURAGE
IMMEDIATE MEDICAL
CARE
Short, mild cramps in a
near term person may be
normal. Contact responsible
school nurse or administrator
& parent or legal guardian.
ENCOURAGE IMMEDIATE
MEDICAL CARE
Contact responsible
school nurse or
administrator & parent or
legal guardian.
ENCOURAGE IMMEDIATE
MEDICAL CARE

Emergency First Aid Guidelines for California Schools Page 61
Other symptoms may indicate that the person
needs medical care. Does the person have:
Abnormal behavior?
Difficulty breathing or swallowing?
Purple spots with fever?
Light-headedness, extreme weakness?
CALL EMS 9-1-1
Contact responsible
school nurse or
administrator & parent or
legal guardian.
If any of the following symptoms are found
in association with a rash, contact
responsible school nurse or administrator
& parent or legal guardian and
ENCOURAGE MEDICAL CARE
Fever (See “Fever”) (pg. 45)
Headache
Diarrhea
Sore throat
Vomiting
Rash is bright red and sore to touch.
Rash (hives) is all over body
If person is so uncomfortable (e.g.,
itchy, sore, feels ill) that he/she is not
able to participate in school activities
YES
NO
RASHES
Rashes may have
many causes,
including heat,
infection, illness,
allergic reactions,
insect bites, dry skin
or skin irritations.
Some rashes may be contagious by direct contact
or respiratory droplets
Wear disposable gloves to protect self when in
contact with any rash.
Rashes may look like:
Hives
Red spots (large or small, flat or raised)
Purple spots
Blisters
See “Allergic Reaction”
(pg. 17) and
“Communicable Diseases”
(pg. 36) for more
information.

Emergency First Aid Guidelines for California Schools Page 62
Is seizure lasting longer than 5 minutes?
Is person having multiple seizures following
one another at short intervals?
Is person having any breathing difficulties
after the seizure?
After seizure, keep airway clear by
placing person on his/her left side
and support the head in a neutral
position with a towel roll
Seizures are often followed by
sleepiness and confusion. This may
last from 15 minutes to an hour or
more
CALL EMS 9-1-1
Contact
responsible
school nurse
or
administrator &
parent or legal
guardian.
During or immediately after a seizure,
place on the floor (preferably a mat) for
observation and safety
DO NOT RESTRAIN MOVEMENTS
Move surrounding objects to avoid injury
Protect head and neck using a jacket or
padding like a folded towel/cloth
DO NOT PLACE ANYTHING
BETWEEN THE TEETH or give
anything by mouth
Note:
Observe details of the seizure for parent or legal
guardian, emergency personnel, or physician.
Duration, movement of eyes, mouth, arms &
legs
Loss of urine/bowel control
Loss of consciousness or change in behavior
After the sleeping period, the
person should return to normal
and be encouraged to
participate in all normal class
activities.
SEIZURES
YES
NO
Refer to person’s Emergency Action/Care
Plan, if available, follow
instructions from person’s guardian or
physician.
A person with a history of seizures
should be known to appropriate
staff.
An emergency care plan should be
developed containing a description of
the onset, type, duration and after
effects of that person’s seizures. If
there is a history of diabetes, check
blood sugar, see “Diabetes” (pg. 37).
Signs & Symptoms of Seizure
Episodes of staring and nonresponsive
Staring with twitching of the arm and/or leg muscles
Generalized jerking movement of arms and/or legs with unconsciousness
Sudden unusual behavior for that person (e.g., strange sounds, belligerence, running)
If trained personnel and medication available, administer Diastat.

Emergency First Aid Guidelines for California Schools Page 63
Any serious injury or illness may lead to shock which is
a lack of blood and oxygen getting to tissue.
STAY CALM and get medical assistance
Shock is a life-threatening condition
Check for medical bracelet or medallion
Lie person down – keep body flat
Control Bleeding: apply direct pressure and see “Bleeding” (pg. 24)
If person vomits, roll on to left side keeping back & neck straight if injury suspected
Minimize pain by position of comfort
Elevate feet 8-10 inches, unless this causes pain/discomfort, OR a neck/back/hip injury
is suspected
Keep body normal temperature, if cold provide blankets. Avoid chilling
NOTHING to EAT OR DRINK
Stay with person and reassure until help arrives. Monitor breathing
Signs of SHOCK
Pale, cool, moist skin
Unresponsive
Generalized weakness
Mottled, ashen, blue skin
Abnormal behavior
Rapid or difficulty breathing
Altered consciousness
Restlessness/irritability
Nausea, dizziness, thirsty
CALL EMS 9-1-1
Is person:
Unconscious? See “Loss of Consciousness” (pg. 53)
Not breathing? See “CPR” (pg. 29)
Look seriously sick? (see signs & symptoms listed
below)
Bleeding profusely? See “Bleeding” (pg. 24)
SERIOUSLY ILL/SHOCK
For Injury
Do Not move
person until extent
of injury is known,
unless
endangered.
YES
NO
Contact responsible
school nurse or
administrator & parent or
legal guardian.

Emergency First Aid Guidelines for California Schools Page 64
.
Is splinter or pencil lead:
Protruding above the surface of skin?
Small and shallow?
Remove with tweezers unless this
causes pain
DO NOT PROBE UNDER SKIN
Contact
responsible
school authority
& parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
Were you successful in removing
the entire splinter/pencil lead?
Wash the area again
Apply clean dressing
Leave in place
DO NOT PROBE UNDER SKIN
Check immunization record for DT, DPT (tetanus).
See “Tetanus Immunization” (pg. 68).
NO
NO
SPLINTERS or IMBEDDED PENCIL LEAD
Wear disposable
gloves when
exposed to blood or
other body fluids.
Gently wash
area with clean
water and soap.
Reassure victim
pencil “lead” is
actually graphite
and does not
cause lead
poisoning.
YES
YES

Emergency First Aid Guidelines for California Schools Page 65
Stomach aches may have many causes including:
Illness
Menstrual difficulties
Hunger
Psychological issues
Overeating
Constipation
Diarrhea
Gas pain
Food poisoning
Pregnancy
Trauma
Have person lie down in a room that affords privacy.
Ask female when last menstrual period was? Is she pregnant? If yes, see “Pregnancy” (pg.59)
If vaginal bleeding, see “Menstrual Problems” (pg. 54)
Has an injury occurred?
Take temperature
Note temperature over 100.0 degrees F as
fever, see “Fever” (pg. 45)
Does person have:
Fever?
Severe stomach pains?
Vomiting?
Allow person to rest for 20-30 minutes.
Is person better?
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
MEDICAL CARE
Allow person
to return to
class/work
Contact responsible
school nurse or
administrator &
parent/legal guardian.
YES
NO
YES
NO
YES
NO
STOMACH ACHES/PAIN
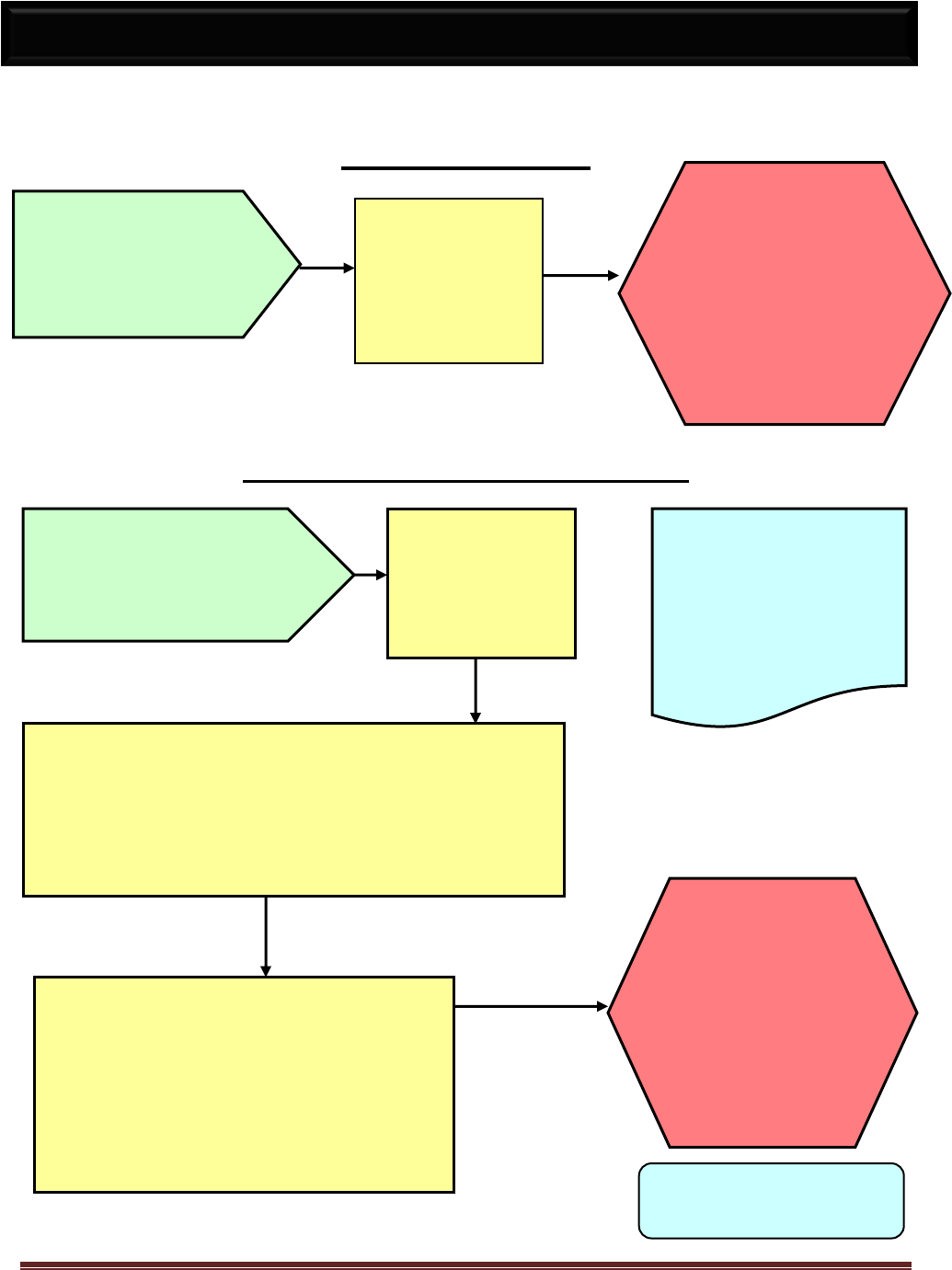
Emergency First Aid Guidelines for California Schools Page 66
BLEEDING GUMS
TOOTHACHE OR GUM ABCESS
A few comfort measures:
If cavities present, a warm salt-
water rinse may remove food
NOTE:
A loose temporary tooth may ache
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
DENTAL CARE
For tongue, cheek,
lip, jaw or other
mouth injury not
involving the teeth,
refer to “Mouth &
Jaw” (pg. 55).
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
ENCOURAGE
DENTAL
CARE
No first aid
measure in the
school will be of
any significant
value.
Relief of pain in the school often postpones dental
care. Administer pain reliever, ibuprofen or
acetaminophen as school protocol allows.
DO NOT place pain relievers (e.g., Aspirin, Tylenol)
on the gum tissue of the aching tooth since they can
cause burns to the tissue!
TEETH CONTINUED ON
NEXT PAGE (pg. 67)
TEETH & GUMS
Generally, related to
chronic infection.
Presents limited threat
to general health.
No first aid
measure in the
school will be of
any significant
value.
These conditions can
affect a person’s general
health, not just local tooth
problems.

Emergency First Aid Guidelines for California Schools Page 67
KNOCKED-OUT TOOTH or Broken Permanent Tooth
DISPLACED TOOTH (Still in Socket)
If a permanent tooth is knocked-out (within 15-20 minutes):
Apply cold compress to face to minimize swelling
If tooth is dirty, hold tooth by crown rinse with water
DO NOT scrub, rub or scrape to remove dirt from tooth
Place in HBSS (Save-A-Tooth Kit) if available, OR
If student is old enough, gently insert and hold the tooth in
its socket, if not possible, place in glass of milk, OR
Have person spit in cup and place tooth in it
Remember to take the tooth with you
TOOTH MUST NOT DRY OUT
For primary (temporary) teeth:
Find Tooth
Do not handle root of tooth
Use Disposable Gloves
Have student bite on folded gauze
to stop bleeding
Place tooth in container or
envelope to take home
Return to normal activities
TEETH (CONT.)
Contact responsible school
nurse or administrator & parent
or legal guardian.
OBTAIN EMERGENCY DENTAL
CARE. A DENTIST SHOULD SEE
THE PERSON WITHIN
60 MINUTES.
DO NOT try to move
tooth into correct
position.
Emergency First Aid Guidelines for California Schools Page 68
Protection against tetanus should be considered with
any wound, even a minor one. After any wound, check
the person’s immunization status for tetanus (DTaP,
Tdap, DPT, DT Td) and notify parent or legal guardian.
Note: Tetanus toxoid is nearly always combined with
diphtheria and pertussis (DPT or TdaP).
A wound would need a tetanus booster if it has been at
least 5 - 10 years since the last tetanus shot or if the
person is 5 years old or younger.
Other wounds, such as those contaminated by dirt,
feces, saliva or other body fluids; puncture wounds;
amputations; and wounds resulting from crushing,
burns, and frostbite need a tetanus booster if it has
been more than 5 years since the last tetanus shot.
TETANUS IMMUNIZATION

Emergency First Aid Guidelines for California Schools Page 69
.
Refer to your school’s policy
regarding the removal of ticks.
Proceed if not in conflict with policy.
Wear disposable gloves when
exposed to blood and other body
fluids.
After removal, wash the tick area thoroughly with soap and water
Wash your hands
Apply a Band-Aid type dressing. If permitted by school policy, use an
antiseptic or antibiotic ointment
Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
Placing ticks in a container of alcohol or flushing
them down the toilet will safely dispose of them.
If any head or mouth parts remain in skin,
ENCOURAGE MEDICAL CARE.
TICKS
Inspect for ticks after
time in woods or brush.
Ticks may carry
serious infections and
must be completely
removed.
DO NOT handle ticks
with bare hands.
Using tweezers grasp the tick as close to the skin surface as possible
and pull upward with steady, even pressure
DO NOT twist or jerk the tick as this may cause the mouthparts to
break off. It is important to remove the ENTIRE tick
Take care not to squeeze, crush, or puncture the body of the tick as
its fluids may carry infection
DO NOT ATTEMPT TO BURN A TICK OFF OR PRICK IT WITH A
PIN

Emergency First Aid Guidelines for California Schools Page 70
If a number of adults and/or
children become ill with the same
symptoms, suspect food
poisoning.
CALL POISON CONTROL
CENTER
1-800-222-1222
Follow instructions.
(See “Poisoning”)
Notify public health (usually
the local County Health
Department).
Phone #_________________
Have a bucket available
Apply a cool, damp cloth to face or forehead
Have person recline or lie down in a position of
comfort in a room that affords privacy
Give no food or medications
Offer ice chips or small sips of clear fluids (e.g.,
water, diluted 7-up, diluted Gatorade) and assess
ability to tolerate fluids
Is person vomiting clots or more than flecks or
streaks of blood? Does person have decreased
level of consciousness?
CALL EMS 9-1-1
Does patient have altered level of
consciousness, pain, and associated fever,
diarrhea, dizziness or lethargy?
See appropriate guidelines.
VOMITING
Contact responsible
school nurse or administrator & parent
or legal guardian.
ENCOURAGE MEDICAL CARE
Vomiting may have many causes including:
Illness or Injury
Food Poisoning
Pregnancy
Heat Exhaustion
Overexertion
Drugs or Alcohol
Toxic Exposure or Ingestion
Near Fainting
Intestinal Illness
If you know the cause of the vomiting see the appropriate
guideline.
Wear disposable gloves when exposed to blood and
other body fluids.
YES
NO

Emergency First Aid Guidelines for California Schools Page 71
Is the Wound:
Large?
Deep?
Bleeding freely?
WOUNDS
(CUTS, SCRATCHES & SCRAPES
INCLUDING ROPE & FLOOR BURNS)
Rinse under running water
Pat dry with clean gauze or
paper towel
Apply clean gauze dressing
(non-adhering/non-sticking
type) and bandage
Use wet gauze or
towel to wash the
wound gently with
clean water and
soap in order to
remove dirt.
Wear disposable gloves when exposed to
blood or other body fluids.
Use direct pressure on the wound to
control bleeding.
Apply direct
pressure on
bleeding site
and see
“Bleeding”
(pg. 24).
Notify parent if
wound is deep,
dirty, gaping or
has embedded
material. Contact
responsible
school nurse or
administrator &
parent or legal
guardian.
Some Signs of Internal Bleeding
Include persistent abdominal pain, rapid-weak
pulse, cool-moist skin, paleness, confusion or
fainting, weakness, vomiting or blood in sputum.
Internal bleeding needs emergency medical
attention.
Refer to primary
care provider as
needed to update
immunizations
against tetanus.
NO
YES

Emergency First Aid Guidelines for California Schools Page 72
Has the eye
been injured?
Is object still visible in
wound?
DO NOT REMOVE OBJECT
Try to calm person
Wash the wound gently with
soap and water
Cover with a clean bandage
Is object large?
Is wound deep?
Is wound bleeding freely or squirting blood?
Is air escaping from wound in the chest?
CALL EMS 9-1-1
See “Bleeding” (pg. 24)
Check person’s immunization record
for DT, DPT (tetanus).
See “Tetanus” (pg. 68) for more
information.
Contact responsible
school nurse or
administrator &
parent or legal
guardian. If more
than a superficial
wound
ENCOURAGE
MEDICAL CARE
DO NOT TRY TO PROBE
OR SQUEEZE
If wound is deep or bleeding
freely, treat as bleeding,
see “Bleeding” (pg. 24).
YES
WOUNDS (PUNCTURE)
Wear disposable
gloves when
exposed to blood or
other body fluids.
Apply direct pressure
to control bleeding.
YES
NO
DO NOT
TOUCH EYE
See
“Eye Injury”
(pg. 42).
NO
NO
YES

Emergency First Aid Guidelines for California Schools Page 73
Is the person:
Pale, sweaty skin?
Losing consciousness?
Having difficulty breathing?
Bleeding uncontrollably?
Open the airway and
look, listen and feel for
breathing, see “CPR”
(pg. 32).
If impaled object, do not remove
Press firmly with a clean bandage to stop
bleeding, see “Bleeding” (pg. 24)
Have person lie down
Elevate feet 8-10 inches
Elevate injured part gently, if possible
Cover with a blanket or sheet
Wear disposable gloves when exposed to
blood or other body fluids.
NO
WOUNDS (STABS & GUNSHOT)
CALL the police via 9-1-1
Tell dispatcher if Emergency Medical
Services are also needed
Intervene only if the situation is safe for
you to approach
Get someone to assist you
Refer to your
school’s policy
for handling
violent
incidents.
Contact responsible
school nurse or
administrator &
parent or legal
guardian.
YES

Emergency First Aid Guidelines for California Schools Page 74
1. Current National American Red Cross First Aid Manual or equivalent.
2. American Academy of Pediatrics First Aid Chart.
3. Portable stretcher
4. Cot: mattress with waterproof cover
5. 10 Triage Tags
6. Blankets, sheets/pillows/pillow cases (disposable covers are suitable)
7. Wash cloths, hand towels, small portable basin
8. Covered waste receptacle with disposable liners
9. Manual resuscitation bag (Ambu bag) [optional]
10. Bandage scissors, tweezers
11. Disposable thermometer or electronic thermometer with disposable covers
12. Sink with running water
13. Expendable supplies (refer to http://www.redcross.org/disaster/masters/supply.html for
recommended inventory):
Pocket mask/face shield for CPR
Disposable gloves (including latex free gloves for persons with a latex allergy)
Soap (plain)
Cotton tipped applicators, individually packaged
Assorted Band-Aids (1”x3”)
Gauze squares (2”x2”’; 4”x4”), individually packaged
Adhesive tape (1” width)
Gauze bandage (2” and 4” widths) rolls
Ace bandage (2” and 4” widths)
Splints (long and short)
Cold packs
Triangular bandages for sling & Safety pins
Tongue blades
Disposable facial tissues
Paper towels
Sanitary napkins
One flashlight with spare bulb and batteries
Hank’s Balanced Salt Solution (HBSS) – Available in the Save-A-Tooth emergency
tooth preserving system or 1/3 cup of powdered milk for dental first-aid (for mixing
with water to make a liquid solution)
Bleach for cleaning contaminated surface
RECOMMENDED FIRST AID EQUIPMENT AND
SUPPLIES FOR SCHOOLS

Emergency First Aid Guidelines for California Schools Page 75
Complete this page as soon as possible, review annually and update as needed. Copy
and post near all phones.
EMERGENCY MEDICAL SERVICES (EMS) INFORMATION
EMERGENCY PHONE NUMBER 9-1-1
Location(s) of Automated External Defibrillator(s) (AED)
Location of First Aid Supplies
BE PREPARED TO GIVE THE FOLLOWING INFORMATION &
DO NOT HANG UP BEFORE THE OTHER PERSON HANGS UP!
Address
Exact location of injured person (e.g., parking lot C, big oak tree)
Provide easy directions to make it easier to find you
School Telephone Number:
o Cell phone number, if applicable
Your name
School name
Nature of Emergency
Other Important Phone Numbers
School Nurse
Responsible School Administrator
Poison Control Center (National)
1-800-222-1222
Suicide Hotline
1-800-273-8255
Fire Department
9-1-1
Police
9-1-1
Hospital or Nearest Emergency Facility
Child Protective Services
Rape Crisis Center
Local Health Department
Other Medical Services Information
(i.e., physicians, urgent care centers, dentists, etc.)
EMERGENCY PHONE NUMBERS
